7 Drugs Whose Dangerous Risks Emerged Only After Big Pharma Made Its Money
Have you ever noticed how warnings about dangerous prescription drugs always seem to surface after the drug is no longer marketed and its patent has run out? Whether it’s an FDA advisory or a trial lawyer solicitation about harm that may have been done to you, the warnings are always belated and useless. If a drug you took four years ago may have given you liver damage, why didn’t the FDA tell you then? Why didn’t the FDA recall the drug or better yet, not approve it in the first place?
The official answer from the FDA and Big Pharma is that problems with a drug are only seen after millions begin using it, which is why post-marketing surveillance is conducted. In other words who knew? But in a startling number of cases revealed in court documents Pharma did“know” and clearly misled medical journals, the FDA, doctors and patients, hoping to get its patent’s worth before the true risks of a drug surfaced. In other cases, Pharma and the FDA should have known before rushing a dangerous drug to market and making money at the expense of patients.
It is the business model for new drugs that provokes Big Pharma to bury risks and exaggerate benefits. A new drug under patent has a high price and no competition, and will make millions or even billions every year it is under patent. A settlement for death or injuries down the road is a nuisance and just the cost of doing business. Needless to say, the “forgiveness is cheaper than permission” business plan breeds shameless repeat offenders since the company makes money and no officers go to jail.
Hidden and unforeseen risks in new drugs are such a danger that some medical professionals advise patients to wait up to seven years before they try a new drug. Of course, the drug is no less risky when made by a generic drugmaker except that it has been in use longer and is not accompanied by slick advertising to push demand and even “sell” the condition it treats. But generics have their downside, too. Unlike branded drug companies, a 2013 Supreme Court ruling says generic drug makers can’t be sued.
Here are some drugs whose risks did not did not keep them from getting their “patent’s worth.”
1. Vioxx: Remember the “super aspirin” Vioxx, that was heavily marketed by Merck and athletes Dorothy Hamill and Bruce Jenner 15 years ago? Vioxx was a wonder drug that treated everything from arthritis pain to menstrual cramps, its ads claimed, sparing users the gastrointestinal problems caused by older drugs like aspirin. It turned out that Vioxx was super at something else, too: it doubled the riskof cardiac events,causing 27,785 heart attacks and sudden cardiac deaths according to news sources.
While Merck pleaded ignorance, the New England Journal of Medicine in 2006 accused Merck of concealing “critical data on an array of adverse cardiovascular events” caused by Vioxx. It was withdrawn in 2004. In 2007, Merck agreed to pay $4.85 billion to patients or survivors’ families which represented less than one year of Merck’s profits, computed the New York Times. Vioxx made Merck an estimated $2.5 billion a year from its 1999 launch to its 2004 withdrawal. Who says crime doesn’t pay?
2. Fosamax: Vioxx was not the only Merck drug demonstrating that forgiveness is easier and cheaper when it comes to marketing new drugs. Merck’s Fosamax, the first of an anti-osteoporosis drug class called biphosphonates that included Boniva and Actonel, was linked to heart problems, intractable pain, jawbone death, bone fractures and esophageal cancer only after its patent ran out in 2008. Court-released documents reveal that Merck scientists knew about Fosamax’ link to jawbone death as early as the 1970s in animal studies.
There was even a subplot to Merck’s mendacity. The company installed bone density scanners in medical offices across the US to scare women into taking Fosamax if their scans revealed thinning bones, reported National Public Radio. The subterfuge of “selling” the disease of thinning bones to sell Fosamax did not make a big dent in sales when it came to light: Fosamax was already off patent.
3. Lipitor:What is the best-selling drug in the history of pharmaceuticals? What made $125 billion in 14 and a half years and as much as $11 billion in a single year? Lipitor, Pfizer’s blockbuster statin drug, owed its success to two factors. It was launched in 1997 when direct-to-consumer drug advertising was just beginning and it harnessed the growing national fear of cholesterol-linked heart attacks. Thanks to Lipitor’s “Know Your Numbers” TV ads and Pfizer reps who saturated medical offices with free samples of the white pills and sometimes lunch, more than 29 million people were prescribed Lipitor.
But in 2012 the same year Lipitor’s patent expired those 29 million people (and millions taking other statins) got a surprise from the FDA. The agency made a label change warning that Lipitor and other statins could cause diabetes, liver injury, muscle damage and memory impairment. Who knew? The quartet of concerns “should not scare people off statins,” said Amy G. Egan, deputy director for safety in the FDA’s Division of Metabolism and Endocrinology Products. Right.
4. Nexium: What is the second bestselling drug, after Lipitor? The Purple Pill. Like statins, Nexium and the other Proton-Pump Inhibitors (PPI) to treat gastroesophageal reflux disease (GERD), became household medications thanks to direct-to-consumer advertising. Before Proton-Pump Inhibitors, people took over-the-counter treatments like Tums or Tagamet when they had heartburn or indigestion. As the afflictions were upgraded into the “disease” of GERD, Nexium made almost $5 billion in the US in one year and the class of PPIs made $13.6 billion in one year, translating into 119 million prescriptions.
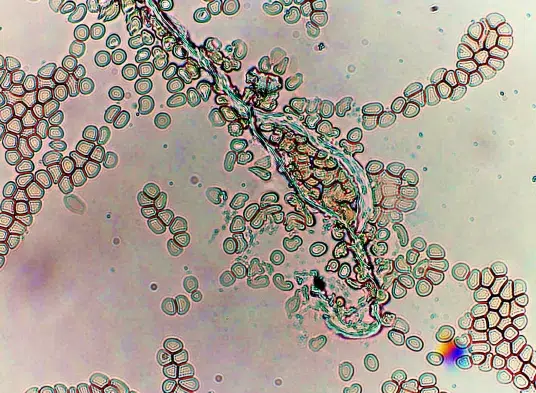
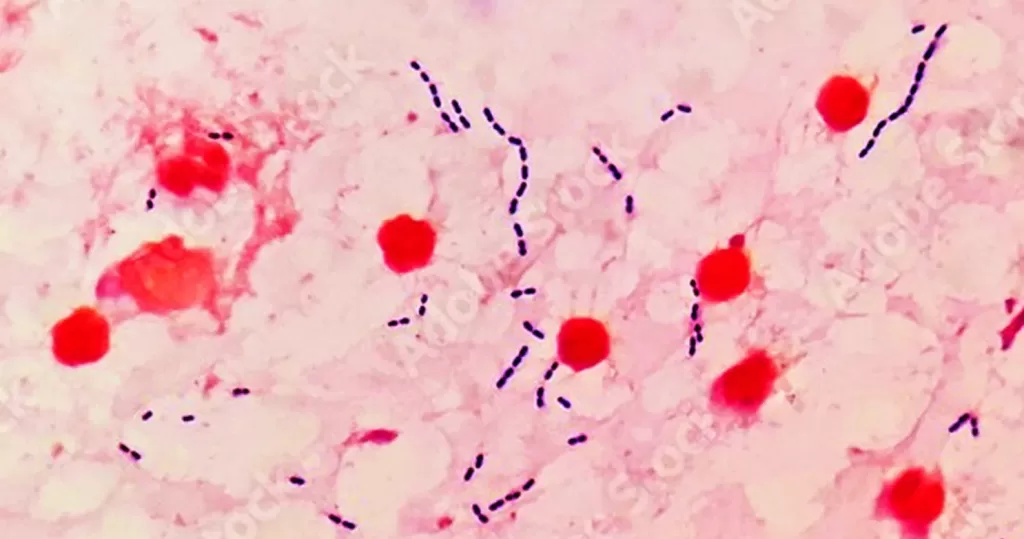
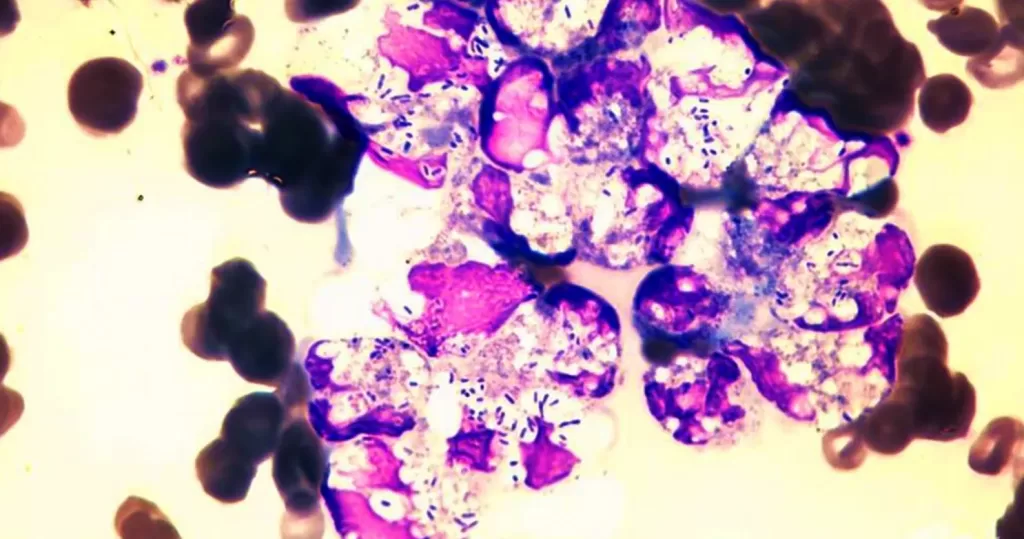
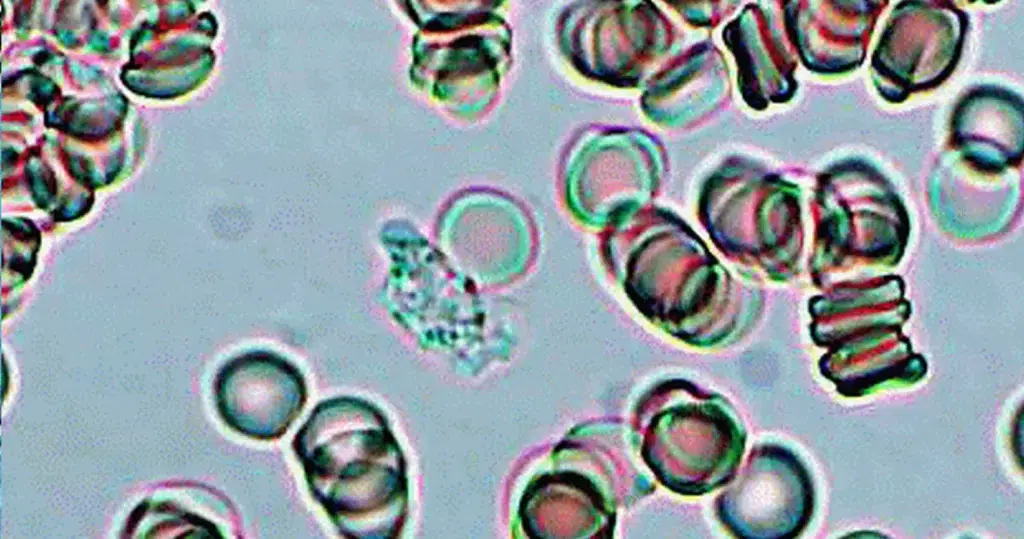
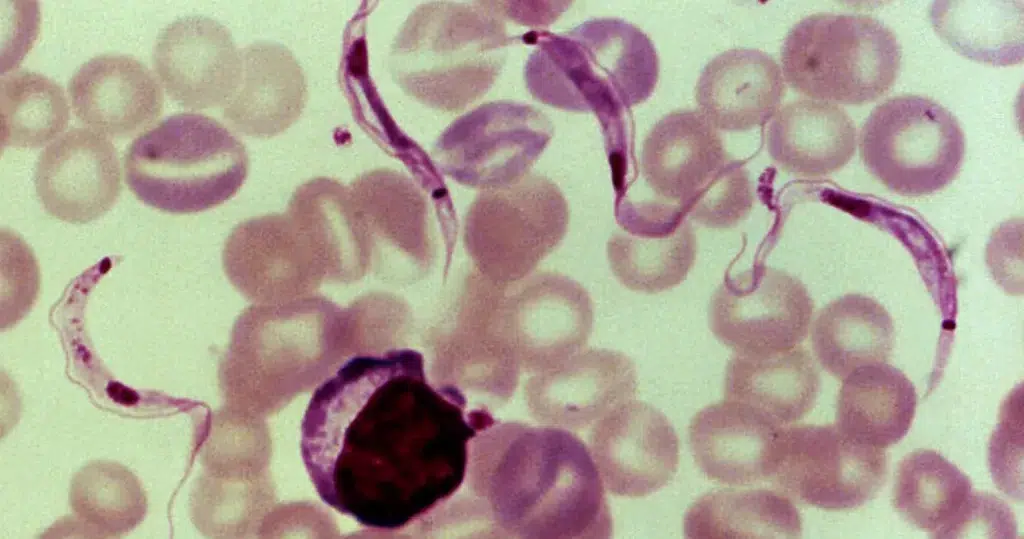
In 2012, the same year the FDA warned about statins, the FDA warned the public that Nexium and the whole class of PPIs are linked to Clostridium Difficile, a stubborn and sometimes deadly intestinal infection that is becoming increasingly drug-resistant and hard to treat. In 2013, medical literature linked PPIs to fractures, calcium and magnesium deficiencies, community-acquired pneumonia and vitamin B-12 deficiencies. Research by John P. Cooke, clinical professor at
Houston Methodist Hospital, found in 2013 that PPIs might cause blood vessels to constrict and cardiovascular risks. Not a great ending for the blockbuster Nexium, whose patent runs out in 2014.
5. Adderall: It is no secret that doctors, parents and teachers are calling millions of children ADHD. Thanks to Pharma marketing, ADHD is now the second most common long-term diagnosis in children after asthma, says the New York Times, often conferred for “childhood forgetfulness and poor grades.” While some critics of the massive dosing say kids are being penalized for being kids and that “treatment” used to be recess, Big Pharma’s spin campaigns maintain that daily stimulants do not hurt children.
But in 2009, the same year Adderall XR went off patent (and two years before Concerta, a time-release version of Ritalin went off patent) a study in the American Journal of Psychiatry found the drugs were actually killing kids. There was “A significant association of stimulant use with sudden unexplained death emerged from the primary analysis,” wrote the authors who looked at 564 cases of sudden death in children 7 to 19. Pro-stimulant Pharma doctors disputed the study, saying the drugs might spare users death by improving their driving skills. Why didn’t anybody test that?
6. Paxil: Few SSRI antidepressants have the checkered safety profile of GlaxoSmithKline’s (GSK) Paxil. In 2007 the BBC revealed that Paxil’s Study 329 showed adolescents six times more likely to become suicidal on the drug but the results were buried. (GSK settled related charges in 2012 for $3 billion.) Rumors had circulated for years about suicide and toxic withdrawal symptoms with Paxil and they were evidently true in some cases.
In 2005, the FDA revealed birth defects associated with Paxil including heart malformations. (Babies may also have “seizures, changing body temperature, feeding problems, vomiting, low blood sugar, floppiness, stiffness, tremor, shakiness, irritability or constant crying,” warned the Paxil website.) Commensurate with the “forgiveness is cheaper than permission” business model, by the time the Paxil risks surfaced, GSK had taken the money and run. In fact, Paxil made $2.12 billion for GSK in 2002, the last year it was under patent, and was the preferred method of treating returning Iraq war veterans’
PTSD.
7. Ambien:One of Big Pharma’s cash cows has been insomnia pills, because everyone watches TV when they can’t sleep and they see sleeping pill ads. Leading the sleeping pill category was Sanofi-Aventis’ Ambien, which netted $2 billion a yearbefore it went off patent in 2006. But even as the patent expired, stories began to circulate about deranged behavior committed in an Ambien blackout. People drove and made phone calls on the drug with no memory of it; dieters woke up amid mountains of pizza and H agen-Dazs cartons, and one woman drank a bottle of black shoe polish in an Ambien blackout. (Sanofi-Aventis was forced to publish ads telling people if they were going to take Ambien, to get in bed and stay there.)
In 2012, the Mayo clinic in Rochester announced it was no longer prescribing Ambien to inpatients because of its fall rate four times that of patients not on Ambien and greater than falls caused by age, mental impairment or delirium. In 2013, the FDA warned about Ambien hangovers, in which the drug has not left the body, and recommended lower doses, especially for women. The warning came too late for Kerry Kennedy, daughter of Robert F. Kennedy and former wife of New York Governor Andrew Cuomo. Witnesses said she had been weaving for miles when she swerved into a tractor-trailer and kept driving, during the summer of 2012. Kennedy told police she may have taken an Ambien thinking it was her daily thyroid med.