The Real “Miracle” Therapy for Vascular Disease
- EDTA chelation may be one of the most effective, least expensive, and safest treatments for heart disease ever developed, yet it is practiced by perhaps only 2,000 physicians in the United States.
- EDTA chelation is not typically covered by medical insurance, even though insurance companies would save billions of dollars each year if they did.
- Although they save far more lives than conventional treatments for heart disease and other chronic degenerative diseases at a fraction of the cost, physicians who practice and promote EDTA chelation for these uses have been harassed, vilified, smeared, and, in some cases, driven from their profession by powerful
medical societies and government agencies that practice and promote conventional medical treatments.
What Is EDTA Chelation?
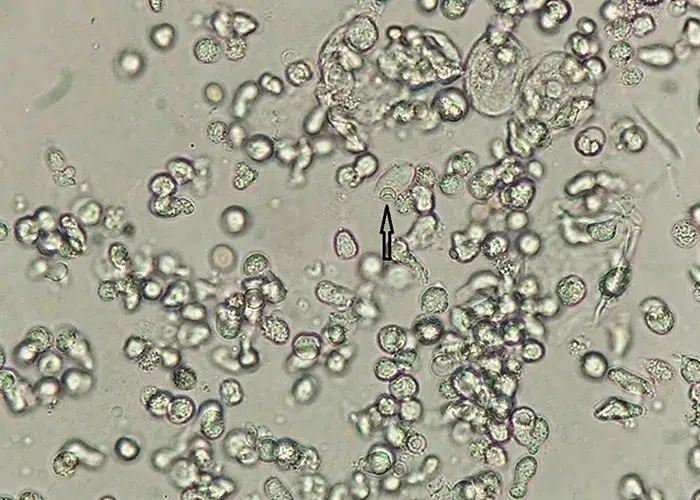
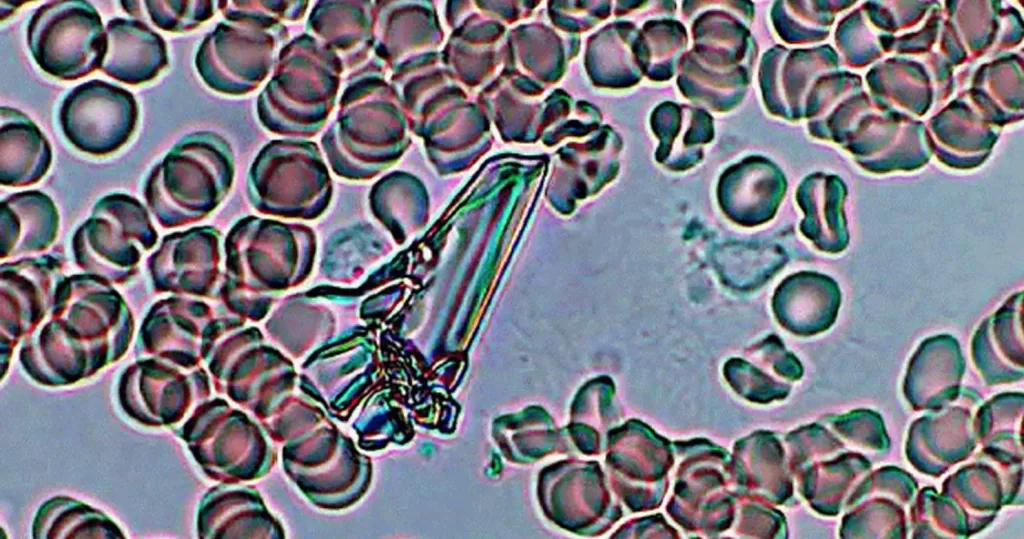
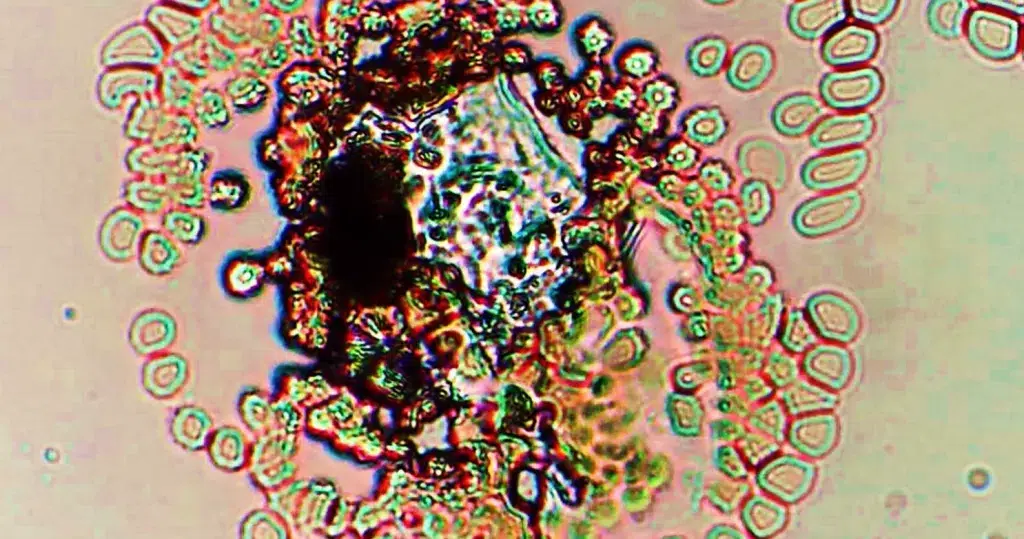
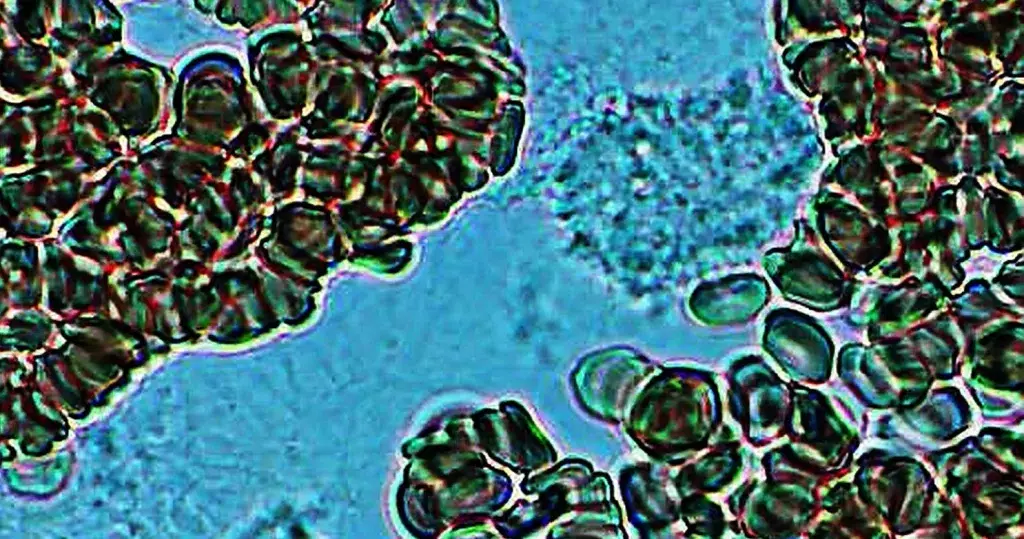
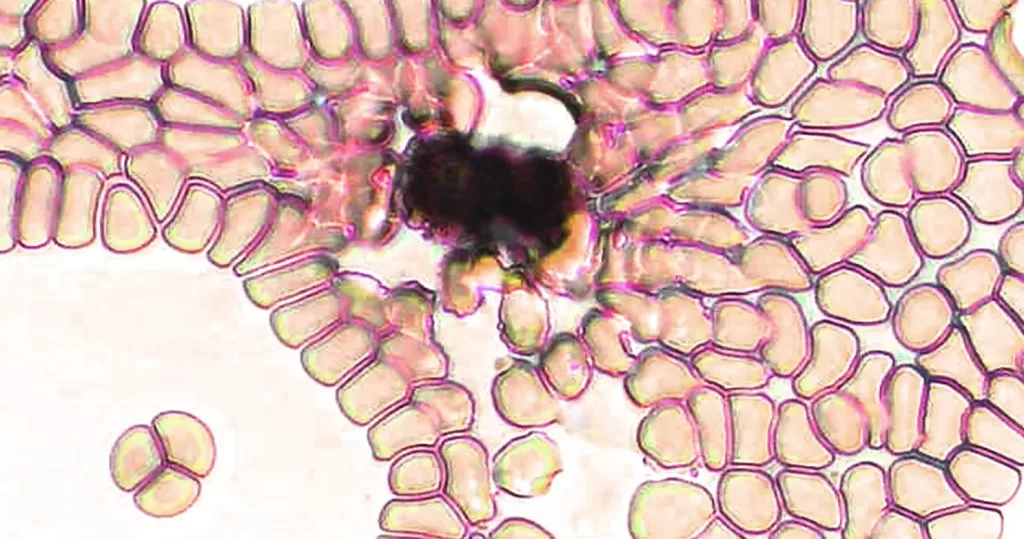
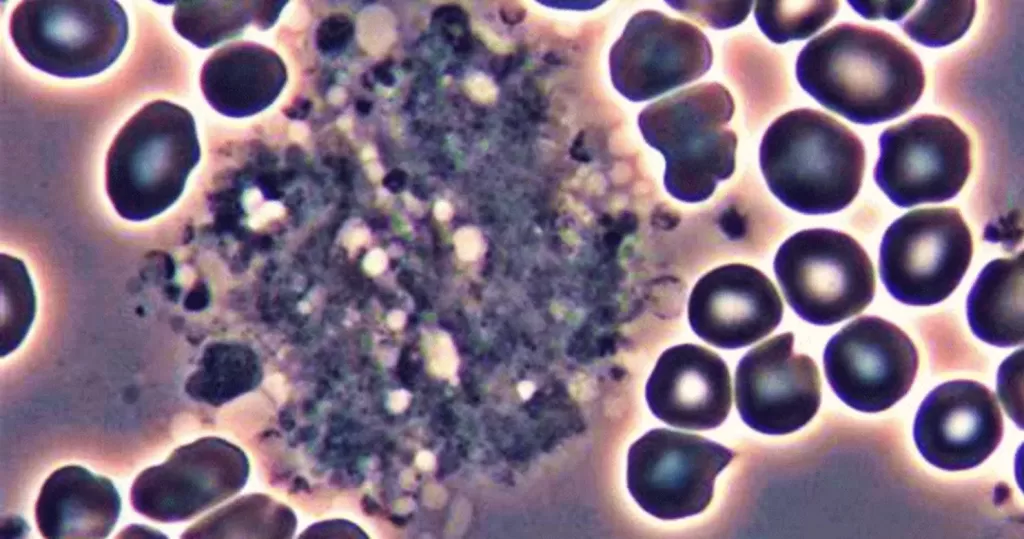
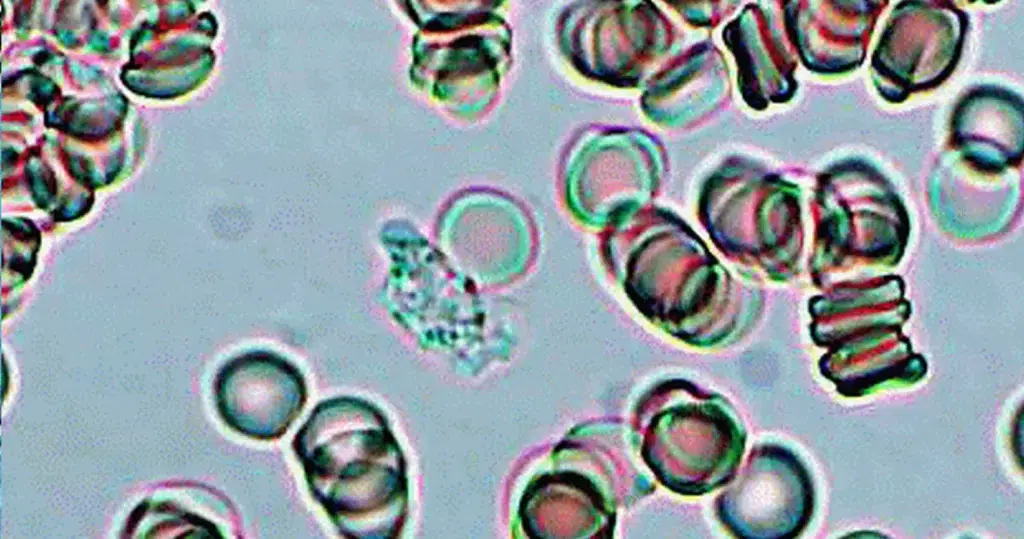
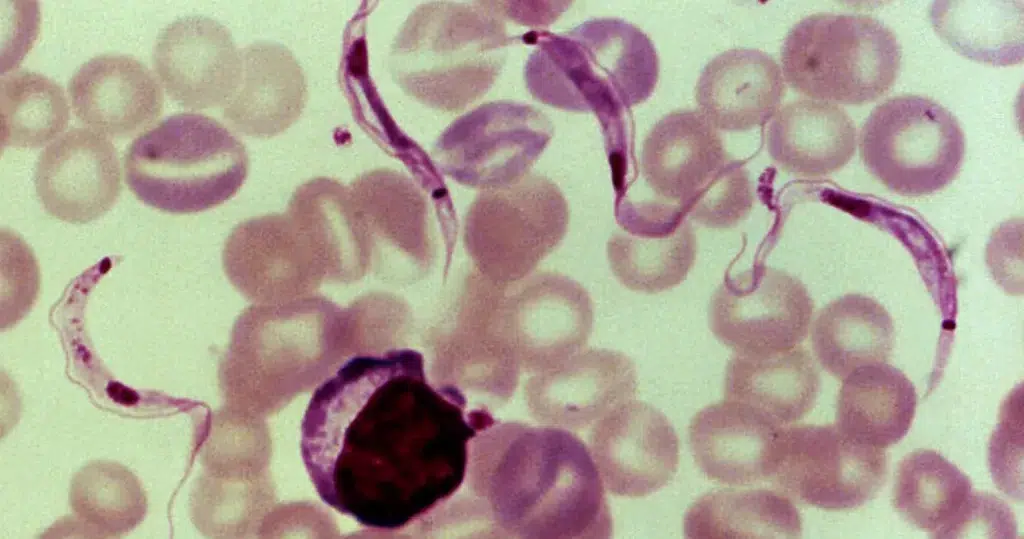
EDTA chelation is a therapy by which repeated administrations of a weak synthetic amino acid (EDTA, ethylenediamine tetra-acetic acid) gradually reduce atherosclerotic plaque and other mineral deposits throughout the cardiovascular system by literally dissolving them away.
EDTA chelation has frequently been compared to a “Roto-Rooter” in the cardiovascular system, because it removes plaque and returns the arterial system to a smooth, healthy, pre-atherosclerotic state. A better metaphor might be “Liquid-Plumr,” because, where Roto-Rooter violently scrapes deposits off the interior surfaces of your plumbing with a rapidly rotating blade, Liquid-Plumr simply dissolves them away.
Roto-Rooter is a far better metaphor for conventional medical treatments for heart disease, all of which are closely tied to the concept of the cardiovascular system as plumbing. When a pipe/artery gets clogged, simply ream it out or flatten the deposits (angioplasty). If that doesn’t work, just cut away the bad section(s) and replace it (them) with a new piece of pipe (coronary artery bypass graft, or CABG). It’s the same basic strategy older cities use for replacing their century-old water mains. And we know how successful that is!
| “Because EDTA is so effective at removing unwanted minerals and metals from the blood, it has been the standard ‘FDA-approved’ treatment for lead, mercury, aluminum and cadmium poisoning for more than 50 years.” |
CABG, known affectionately in the medical profession as “cabbage,” is the most frequently performed surgery in the United States. At up to $50,000 per procedure, that indeed amounts to a lot of “cabbage,” not only for cardiac surgeons but also for hospitals. As we shall see, these figures provide a powerful incentive for physicians to reject an effective, but inexpensive and unpatentable treatment like EDTA chelation.
It is commonplace for physicians who regularly prescribe EDTA chelation to encounter heart disease patients who have failed all the standard treatments but who make remarkable – even unbelievable – recoveries once given EDTA. Other patients, on waiting lists for CABG surgery, found they did not need the surgery following a series of EDTA chelation treatments.
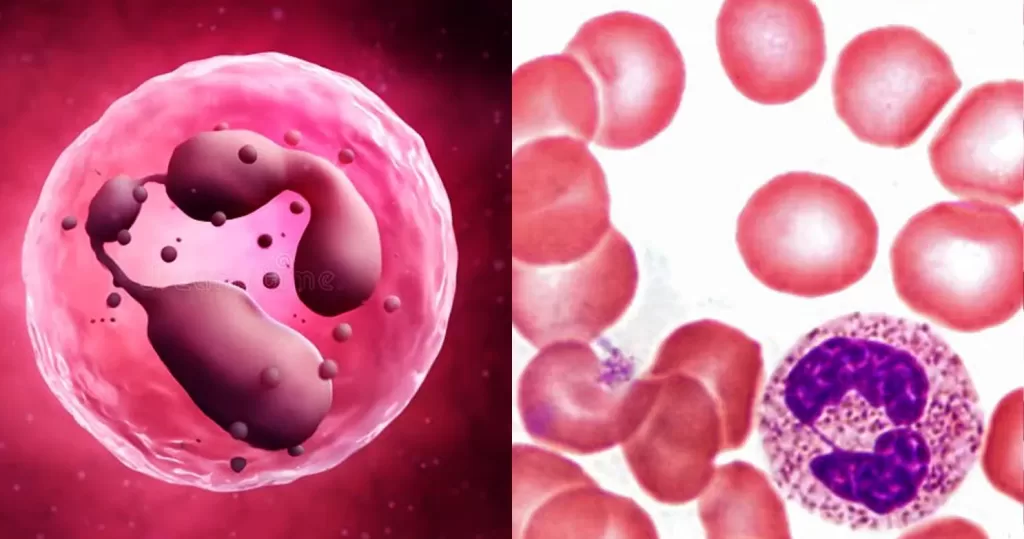
EDTA exerts its beneficial effects on the body because this molecule is extremely proficient at chemically bonding with mineral and metal ions. This bonding process, known as chelation, is a natural and essential physiologic process that goes on constantly in the body. EDTA’s chelating abilities make it ideal for many tasks:
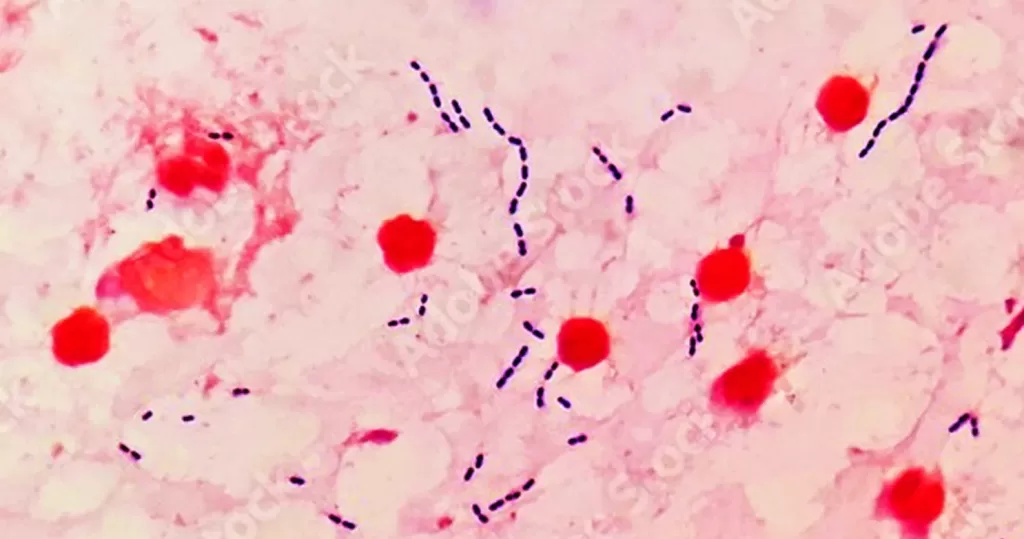
- Because EDTA is so effective at removing unwanted minerals and metals from the blood, it has been the standard “FDA-approved” treatment for lead, mercury, aluminum and cadmium poisoning for more than 50 years. EDTA normalizes the distribution of most metallic elements in the body.
- Because it is so safe and effective, EDTA is also used widely as a stabilizer for packaged food. Minute amounts of EDTA (33-800 PPM) added to food help to preserve flavor and color and to retard spoilage and rancidity. (Read your food labels.)
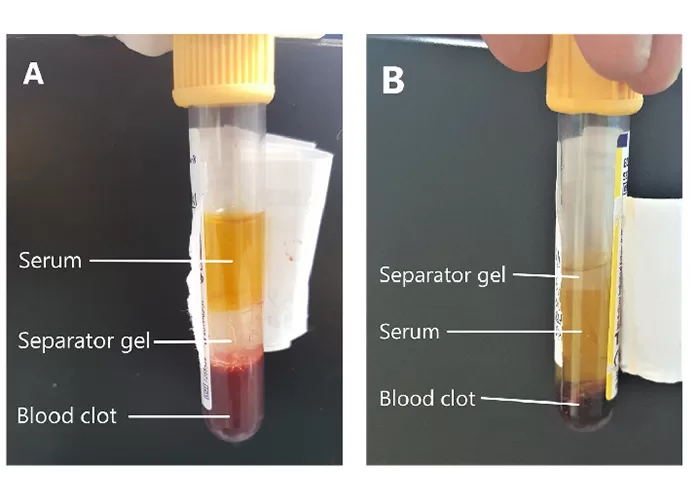
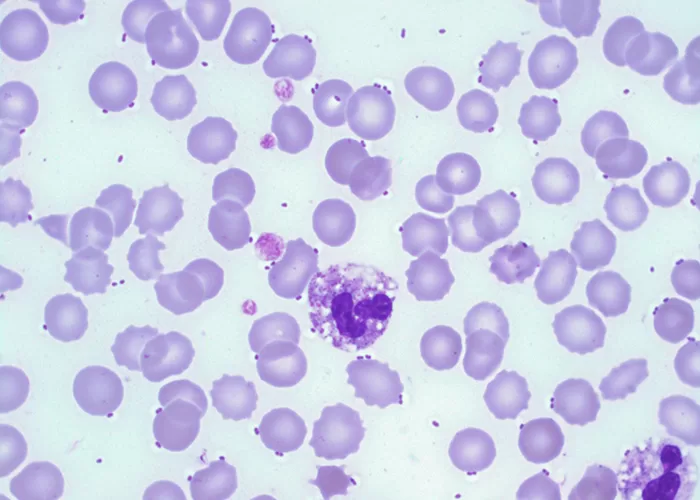
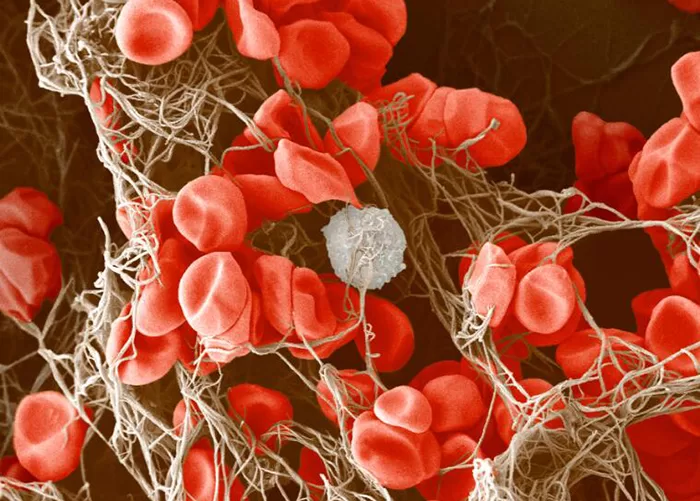
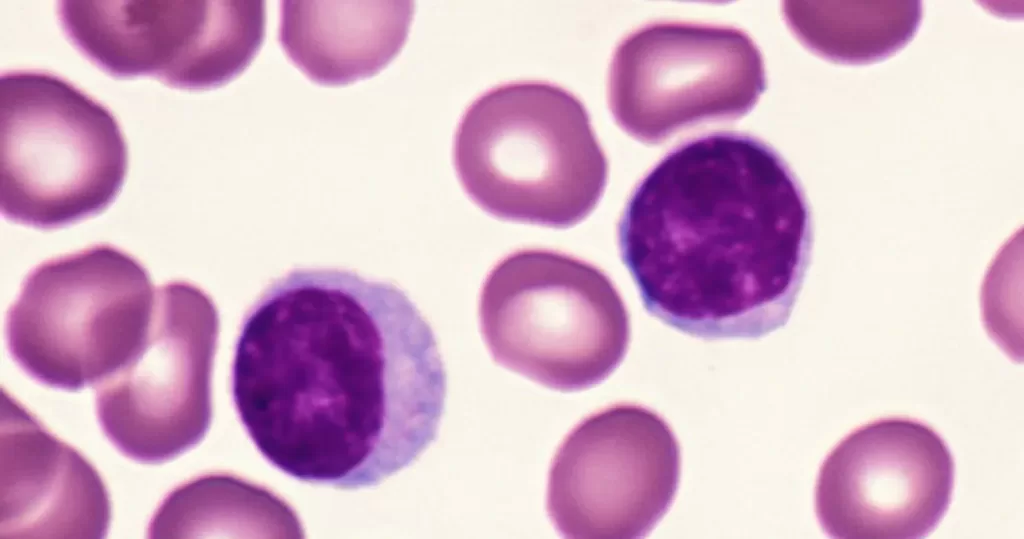
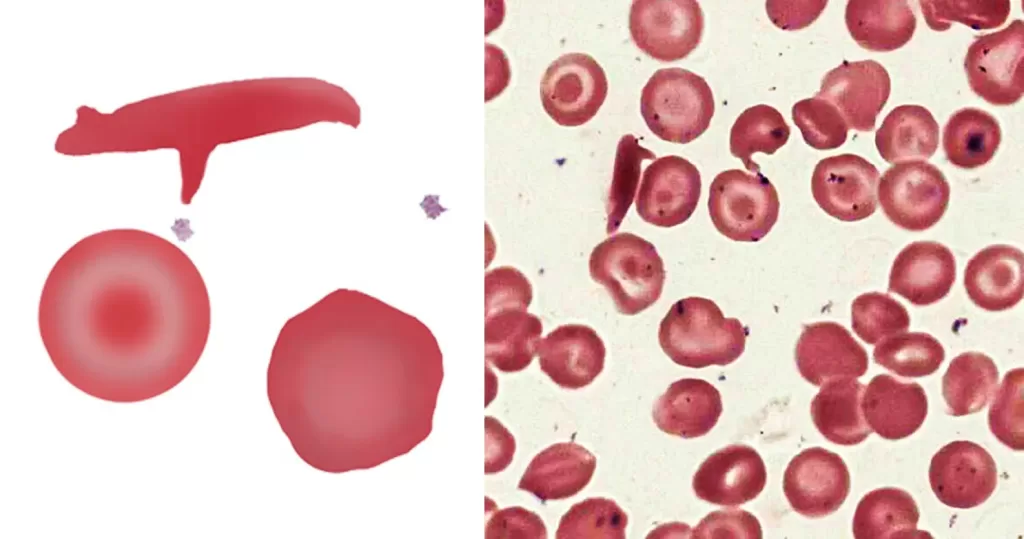
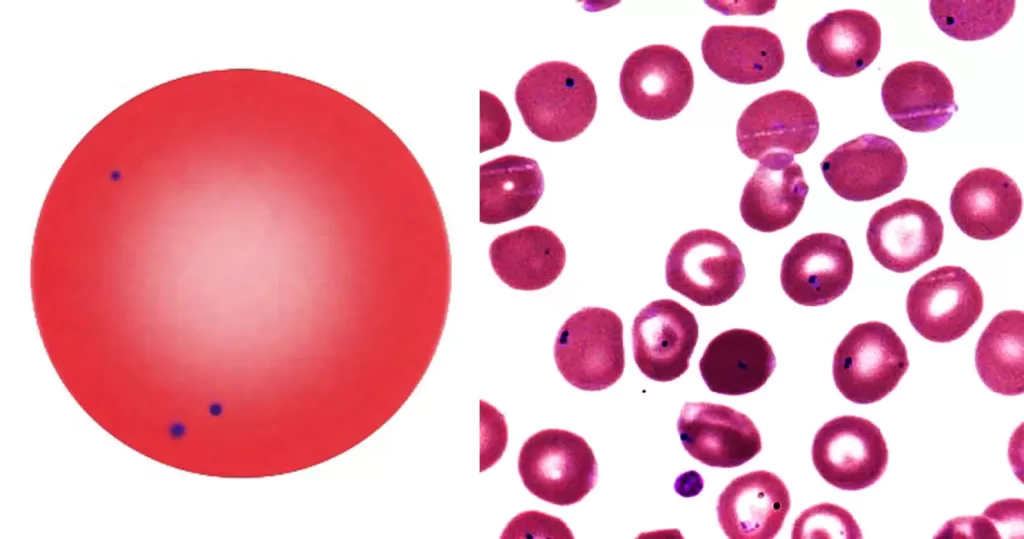
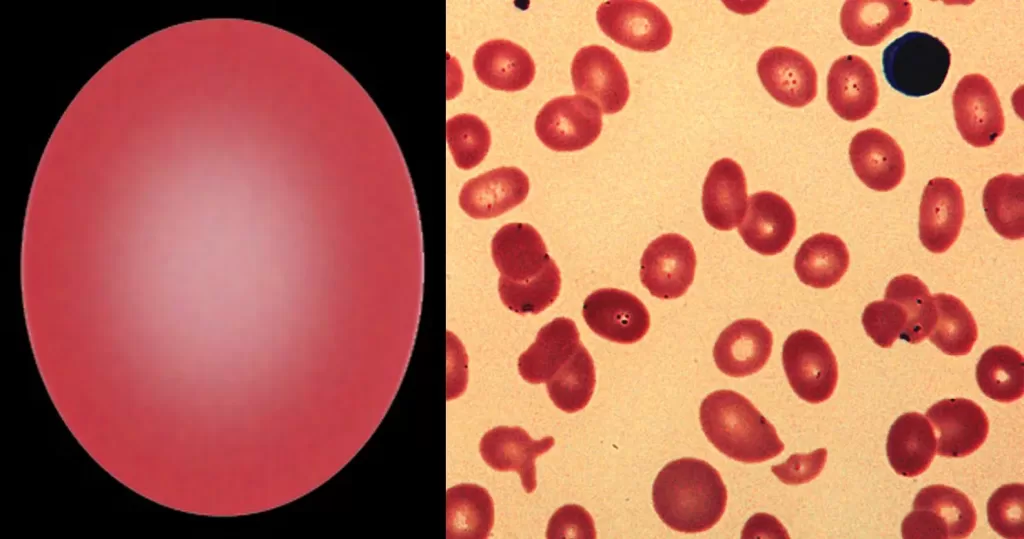
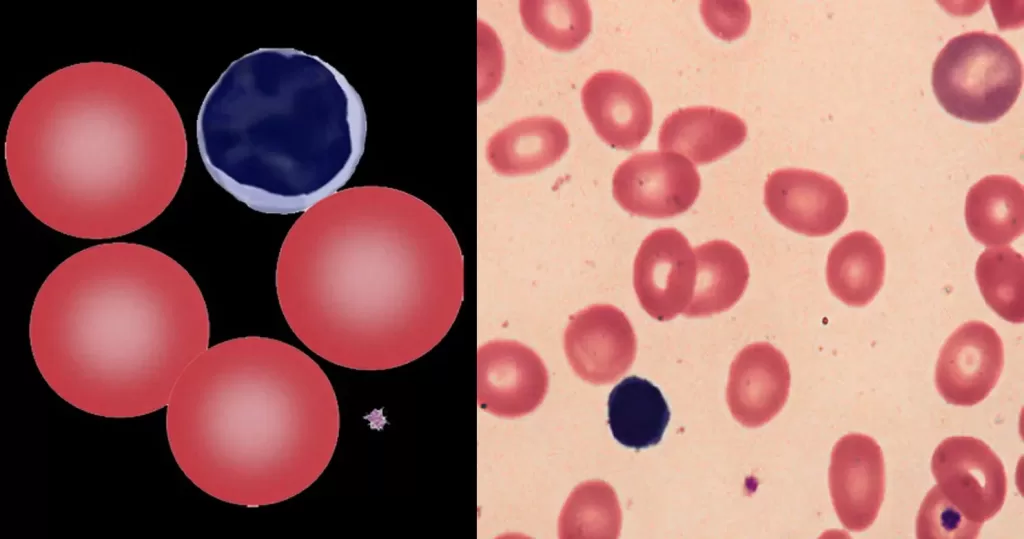
- Because EDTA inhibits blood clotting so well, it is routinely added to blood samples that are drawn for testing purposes.*
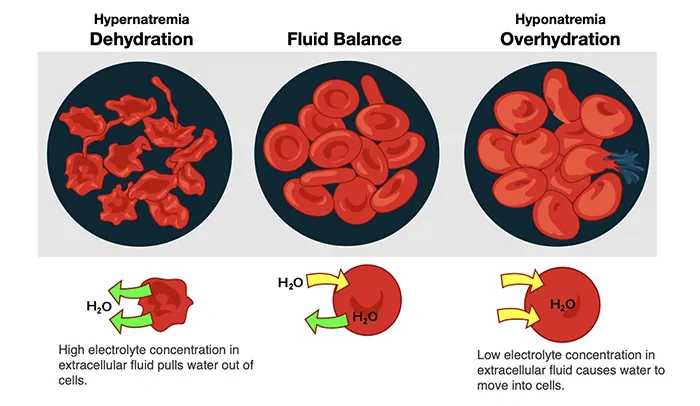
- EDTA improves calcium and cholesterol metabolism by eliminating metallic catalysts that can damage cell membranes by producing oxygen free radicals.
Thanks to these and probably other effects of EDTA, it has been reported to have a wide variety of benefits.
*If you followed the O.J. Simpson trial, you probably know that EDTA was featured prominently. The defense contended that EDTA, supposedly found in certain of “The Juice’s” blood drops at the murder scene, indicated that that blood had spent some time in a collection tube before being “planted” by the LAPD. If there
was EDTA in Simpson’s blood, though, it may well have come from the meal he ate on the plane ride from Chicago to LA.
EDTA Chelation vs. Conventional Therapy for Vascular Disease
Researchers first started to notice EDTA in the days during and after World War II when men who worked in battery factories or painted ships with lead-based paint began coming down with lead poisoning from their high exposure in these jobs. EDTA was found to be extremely effective for removing the lead from the men’s bodies, but what really made people sit up and take notice was an apparent reduction in symptoms of heart disease in many of these men. The first systematic study of EDTA in people with atherosclerosis was published in 1956.1 When the researchers gave 20 patients with confirmed heart disease a series of 30 I.V. EDTA treatments, 19 of the patients experienced improvement, as measured by an increase in physical activity. Another study 4 years later in a similar population found that 3 months of EDTA infusions resulted in decreases in the severity and frequency of anginal episodes, reduced use of nitroglycerin (a common anti-angina
drug), increased work capacity and improved ECG (electrocardiogram) findings.
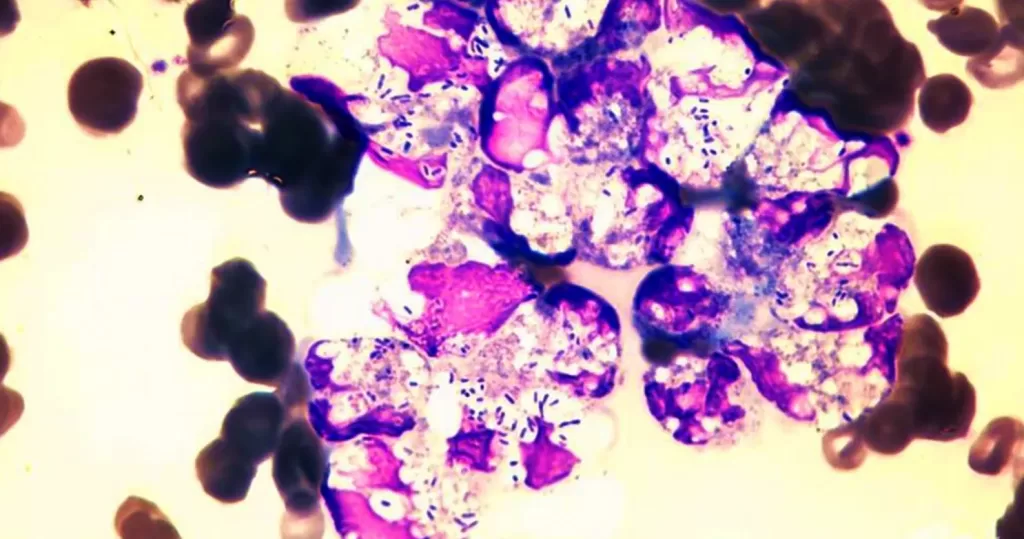
2 It soon became clear from these and later studies that EDTA treatments result in progressive and widespread improvement and stabilization of cardiovascular function. This is in contrast to standard treatments, such as angioplasty or CABG, which instantaneously restore normal function in the few treated arteries, but leave the rest of the body completely untreated (there’s every reason to believe that if arteries are clogged in the heart, they’re also clogged in other vital organs,
like the kidneys and brain). High-tech treatments for heart disease, such as angioplasty and CABG, long hailed as medical breakthroughs, are in fact, oversold, overpriced, and ineffective, especially when compared with EDTA chelation. The truth of this assertion has been demonstrated on numerous occasions over the last 2 decades:
- The average mortality for CABG surgery is 4% to 10%.3,4 In fact, CABG has no overall effect on improving survival. According to one study published in the New England Journal of Medicine, “As compared with medical therapy, coronary artery bypass surgery appears neither to prolong life nor to prevent myocardial infarction in patients who have mild angina or who are asymptomatic after infarction in the five-year period after coronary angiography.”5
By contrast, mortality rates for EDTA chelation, when carried out according to accepted protocols, approaches 0%.6 - Grafted coronary arteries are more than 10 times as likely to close up again within 3 years compared with coronary arteries that are not replaced with a graft.7
Improved blood flow following EDTA chelation therapy is permanent as long as regular EDTA therapy (either oral or I.V.) is maintained. - Significant cerebral dysfunction, especially in older patients, is commonly seen following CABG.8 Because EDTA chelation restores blood flow to the brain, it often results in improved cognition and memory.9
- Atherosclerosis is typically a body-wide disease. If your coronary arteries are occluded, it’s a safe bet that arteries in your brain, kidneys, lungs, and other vital organs are also occluded. Angioplasty or CABG can clean out only a few arteries supplying the heart. Another surgical procedure, endarterectomy, is commonly used to clear out the carotid arteries that supply the brain. When patients who have undergone carotid endarterectomy are treated with EDTA afterwards, the degree of subsequent restenosis (re-occlusion) drops by 10%.10
- Despite the danger and costs associated with these procedures, they are often only temporary fixes. Restenosis of treated coronary arteries occurs within 6 months in as many as one in three cases.11 By contrast, EDTA chelation permanently removes blood vessel obstructions throughout the body without dangerous and expensive surgery. How well does EDTA chelation work? Virtually every study that has looked at the efficacy of EDTA chelation in vascular
disease has demonstrated significant improvements. Here is a brief sampling of a few of the major results: A 1993 meta-analysis of 19 studies of 22,765 patients receiving EDTA chelation therapy for vascular disease found measurable improvement in 87%.12 - In a study of 2,870 patients with various degrees of degenerative diseases, especially vascular disease, almost 90% of the patients showed excellent improvement, as measured by walking distance, ECG, and Doppler changes.13 A small, blinded, crossover study of patients with peripheral vascular disease found significant improvements in walking distance and ankle/brachial blood flow.14
- In 30 patients with carotid artery stenosis, there was a 30% improvement in blood flow after EDTA treatment.15 Using retinal photographs in patients with macular degeneration, one researcher demonstrated significant improvement following EDTA treatment.16
- EDTA chelation treatment was evaluated in patients with carotid and coronary disease using technetium 99 isotope techniques. Significant improvement in arterial blood flow and ejection fraction a measure of heart pumping ability) was reported.17,18
- When 65 patients on the waiting list for CABG surgery for a mean of 6 months were treated with EDTA chelation therapy, the symptoms in 89% (58) improved so much they were able to cancel their surgery. In the same study, of 27 patients recommended for limb amputation due to poor peripheral circulation, EDTA chelation resulted in saving 24 limbs.19
Negative Results?
Of course there have been a few studies that did not (at first) seem to support the efficacy of EDTA chelation therapy. The most prominent apparently well-controlled studies have been two Danish trials 20,21 and a New Zealand trial,22 all of which reported no apparent benefits. A close analysis of these studies, however, revealed problems with both the controls and the interpretation of the data.
| “Because EDTA chelation restores blood flow to the brain, it often results in improved cognition and memory.” |
As noted by Chappell and Janson,6 the standard EDTA chelation treatment protocol was not followed in these trials. They all included primarily smokers (notoriously poor responders) with severe vascular disease who received only 20 I.V. treatments. With such patients, 30 to 40 treatments are normally required before a significant effect is typically seen. Although the New Zealand trial was supposedly placebo-controlled, the “placebo” used actually had chelating properties of its own. Thus, the fact that the differences from “placebo” were small is meaningless.
When the raw data from the New Zealand study were examined, it was found that 26% of the EDTA-treated patients compared with only 12% of the “placebo” controls achieved an improvement of greater than 100% in walking distance; among nonsmokers or smokers who had quit, 66% of the EDTA-treated group increased their walking distance an average of 86% compared with 45% of the controls, who improved by just 56%. Reduced blood flow, as measured by the ankle/brachial index, was found in 6% of the EDTA-treated patients and 35% of the controls. Although the authors of these studies reached negative conclusions, in
fact, their data actually supported the use of EDTA chelation.
How Safe Is EDTA Chelation?
EDTA, is a safe, nontoxic substance. The LD50 (so called when the dose will kill 50% of experimental animals) for EDTA is 2000 mg/kg body weight, which makes it about 3.5 times less toxic than aspirin. Although the FDA refuses to approve it for treating vascular disease, EDTA chelation has been the approved treatment for lead or other heavy metal poisoning for 50 years. When administered according to the treatment protocol developed by the American College for Advancement
in Medicine (ACAM), I.V. chelation is more than 300 times safer than CABG surgery. Most side effects of treatment involve minor discomfort (eg, nausea, dizziness, headache) that resolves quickly.
The greatest risks occur when an infusion is given too rapidly or in too large a dose. These risks virtually vanish when EDTA is administered by a properly trained physician who follows the ACAM protocol. To the extent that oral EDTA is a completely noninvasive therapy, it is even safer than I.V. EDTA.
I.V. or Oral EDTA?
Most chelation therapy carried out today involves I.V. administration of EDTA, however, oral EDTA, which has a history at least as long as its I.V. cousin, is an option that is only now starting to be appreciated. Clinical experience suggests that oral chelation provides some, but not all, of the benefits of I.V. therapy. Overall, the difference in benefits is more one of degree and speed than of quality.
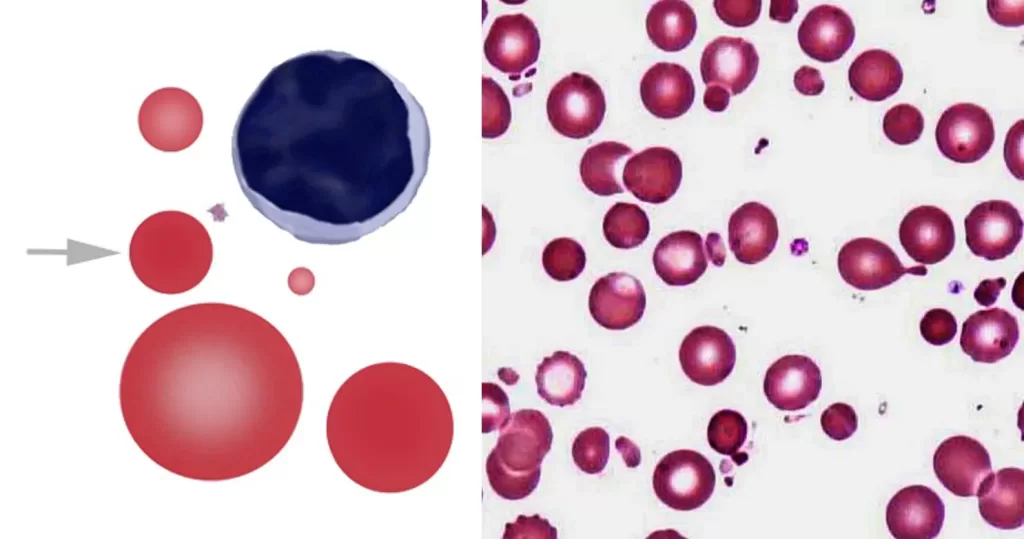
I.V. therapy has a direct and powerful effect on the body almost instantaneously. An I.V. session usually lasts about 3 to 4 hours, during which about 1500 mg to 3000 mg of EDTA (plus vitamin C and other nutrients) are administered. The number of treatments necessary (generally about 20-50 sessions) depends on the individual’s condition. Candidates for I.V. chelation are people that have been diagnosed with serious atherosclerosis, heavy metal poisoning, or symptoms of vascular occlusion or significant calcification of tissues. Only about 3% to 8% of an oral dose of EDTA is absorbed, compared with 100% of an I.V. dose. Therefore, the time and dosage required to achieve the same benefits with the oral form are quite different. What can be achieved in only a few hours with I.V. EDTA
chelation may take several weeks or months with oral EDTA chelation. However, oral EDTA may be appropriate for people whose condition does not demand rapid action. For example, oral chelation can be used to:
- avoid complications and diseases that result from heavy metals and calcification
- prevent the formation of blood clots, thus reducing your chance of a heart attack or stroke
- lower the level of blood cholesterol
- help thin the blood
- aid in reducing lipid peroxidation, a major cause of atherosclerosis
- protect the body against certain carcinogens, pathogens and other toxins that can reduce the quality of health
Oral EDTA is not meant to replace I.V. therapy for those people who have serious vascular disease. It is very useful, though, for people who have completed an I.V. course and want to stay on a maintenance program, for people who “for whatever reason” are unable or unwilling to undergo I.V. chelation, and for those whose I.V.
treatments may have been interrupted.
The Politics of EDTA Chelation
Organizations like the American Heart Association and the American Medical Association, which condemn EDTA chelation as ineffective for treating vascular disease, often quote the Danish and New Zealand studies, mentioned earlier, to support their position.20-22 What they fail to mention is that the Danish studies were criticized by the Danish Committee for Investigation into Scientific Dishonesty because of improper randomization and double-blinding, as well as premature breaking of the blinding code, which amounted to a deliberate bias. When the results of the New Zealand study were examined by two independent statisticians, it was concluded that the trial actually supported the efficacy of EDTA.23
| “Virtually every study that has looked at the efficacy of EDTA chelation in vascular disease has demonstrated significant improvements.” |
It is unlikely that any other issue in modern medicine has been more highly politicized than that of EDTA chelation therapy, and it is clear that most of the opposition to EDTA is due to the threat this therapy represents, not to patients’ health but to the bank balances of orthodox physicians, pharmaceutical companies, and hospitals. Treating cardiovascular diseases is big business in the United States (and the rest of the Western world), bringing in tens of billions of dollars each year.
As Garry Gordon, MD, DO, the “Father of Chelation Therapy” has pointed out, “Every time a surgeon does a heart bypass, he takes home a luxury sports car.” Each CABG procedure costs between $25,000 and $50,000; each angioplasty costs about $15,000; drugs for reducing cholesterol, lowering high blood pressure, and
normalizing heart rhythm bring the pharmaceutical industry hundreds of millions of dollars each year. And these are just the most common examples. What happens when you add EDTA chelation therapy to this mix?
A course of I.V. EDTA chelation therapy costs between $2000 and $4000; oral EDTA is even less costly. To the degree that these therapies reduce the need for the more expensive conventional therapies – a large degree, indeed – they threaten to diminish the income of a significant portion of the medical establishment. Consider
this one example: As noted earlier, in a study of 65 patients who were treated with I.V. EDTA while they were waiting for CABG surgery, 58 (89%) no longer required the procedure.19 At $50,000 per procedure not done, that means that surgeons and hospitals gave up nearly $3 million just for these few patients. Now remember, that CABG is the most common surgical procedure performed in the US (368,000 in 1989).24 Given these figures, it’s not hard to understand why the medical
profession is so in love with CABG and related procedures. As one physician noted, “It pays the bills.” So enamored are they of these procedures that they perform them even when they are not necessary. In an article published in no less prestigious a publication than the Journal of the American Medical Association,
the authors concluded that only 56% of the surgeries performed were for appropriate reasons, 30% for equivocal reasons, and 14% for inappropriate reasons. The percentage of appropriate surgeries varied from 37% in some hospitals to 78% in others.25
When you consider that even when it is “appropriate,” CABG surgery is no better than conventional medical treatments for improving survival,5 you have to wonder whether the real “miracle” of heart surgery does not entail bringing people back from death’s door, as much as turning a common chronic degenerative disease into a source of outrageous fortune. If you needed one example of why the cost of health care has gone into earth orbit, you need look no further than the conventional treatment of heart disease.
| “If you needed one example of why the cost of health care has gone into earth orbit, you need look no further than the conventional treatment of heart disease.” |
Given these figures, it’s also not very hard to understand why the medical profession has reacted so violently against physicians who practice chelation therapy, often attempting, in the words of that great seeker of medical truth (that’s a joke folks), Dr. Victor Herbert, “to put them out of business.” Because EDTA has long been approved for treating heavy metal poisoning, and because physicians are free to use any “approved” medication for any use they see fit, as long it does not endanger the patient, EDTA chelation therapy is perfectly legal. This has not stopped medical boards in a number of states from bringing charges against physicians who prescribe EDTA chelation for vascular disease, smearing them as “quacks,” and attempting to restrict the use of this therapy. Fortunately, most of these attempts have failed.23 You can be certain that if EDTA had a large pharmaceutical company advocating its use, these problems wou quickly evaporate. But since the patent for EDTA ran out nearly 30 years ago, there are no huge profits to be made from marketing it. With no pot of gold at the end of the EDTA rainbow, no one is going to put up the hundreds of millions of dollars required to do the randomized, double-blind, placebo-controlled clinical trials required to get the FDA to approve EDTA for vascular disease. And with few large, randomized, double-blind, placebo-controlled clinical trials to refer to, the conventional medical establishment feels justified in condemning EDTA therapy as “unproven.” It’s a familiar “Catch 22” that faces all natural or unpatentable therapies.
Conclusion
While most American physicians choose to remain blind to the benefits of EDTA, those who prescribe it are free to witness its life-enhancing benefits on a daily basis. One of those physicians is Dr. Garry Gordon, whose own life was saved by EDTA and who has been a leader in chelation therapy since the early 1960s. “I have taken on patients who were inoperable, who had already had every known form of bypass surgery, who had no more veins in their legs to strip out and put into their heart, and who were sent home to die, and I could get those people back to full functioning,” says Dr. Gordon.
| For an interview with Dr. Garry Gordon, see Exclusive Interview with Garry Gordon, M.D., D.O.: Oral Chelation for Improved Heart Function – Apr. 1997 |
POTENTIAL BENEFITS OF EDTA CHELATION
| Prevents cholesterol deposits Reduces blood cholesterol levels Lowers high blood pressure Avoids by-pass surgery Avoids angioplasty Reserves digitalis toxicity Removes calcium from atherosclerotic plaques Dissolves intra-arterial blood clots Normalizes cardiac arrythmias Has an anti-aging effect Reduces excessive heart contractions Increases intracellular potassium Reduces heart irritability Improves heart function Removes mineral and drug deposits Dissolves kidney stones Reduces serum iron levels Reduces heart valve calcification Reduces varicose veins |
Heals calcified necrotic ulcers Reduces intermittent claudication Improves vision in diabetic retinopathy Decreases macular degeneration Dissolves small cataracts Eliminates heavy metal toxicity Makes arterial walls more flexible Prevents osteoarthritis Reduces rheumatoid arthritis symptoms Lowers diabetics’ insulin needs Reduces Alzheimer-like symptoms Reverses senility Reduce stroke/heart attack after-effects Prevents cancer Improves memory Reverses diabetic gangrene Restores impaired vision Detoxifies snake and spider venoms Adapted from: Walker M., Gordon G., Douglass W.C. The Chelation Answer |
http://nukeprofessional.blogspot.com/2012/04/geiger-counter-interpretation.html
References
1. Clarke NE, Clarke CN, Mosher RE. Treatment of angina pectoris
with disodium ethylene diamine tetraacetic acid. Am J Med Sci.
1956;December:654-666.
2. Meltzer LE, Ural E, Kitchell JR. The treatment of coronary artery
heart disease with disodium EDTA. In: Seven M, ed. Metal-Binding in
Medicine. Philadelphia: JB Lippincott; 1960.
3. Edmunds LH, Stephenson LW, Edie RN, Ratcliffe MB. Open-heart
surgery in octogenarians. N Engl J Med. 1988;319:131-136.
4. CASS Principal Investigators and the Associates. Coronary artery
surgery study (CASS): a randomized trial of coronary artery bypass
surgery: Survival data. Circulation. 1983;68:939-950.
5. CASS Principal Investigators and the Associates. Myocardial
infarction and mortality in the Coronary Artery Surgery Study
randomized trial. N Engl J Med. 1984;310:750-758.
6. Chappell LT, Janson M. EDTA chelation therapy in the treatment of
vascular disease. J Cardiovasc Nurs. 1996;10:78-86.
7. Cashin WL, Sanmarco ME, Nessim SA, Blankenhorn DH. Accelerated
progression of atherosclerosis in coronary vessels with minimal
lesions that are bypassed. N Engl J Med. 1984;311:824-828.
8. Arom KV, Cohen DE, Strobl FT. Effect of intraoperative intervention
on neurological outcome based on electroencephalographic monitoring
during cardiopulmonary bypass. Ann Thorac Surg.
1988;48:476-483.
9. Olszewer E, Carter JP. EDTA chelation therapy in chronic
degenerative disease. Med Hypotheses. 1988;27:41-49.
10. Holliday HJ. Carotid restenosis: A case for EDTA chelation. J
Adv Med. 1996;9.
11. Parisi AF, Folland ED, Hartigan PA. Comparison of angioplasty with
medical therapy in the treatment of single-vessel coronary artery
disease. N Engl J Med. 1992;326:10-16.
12. Chappell LT, Stahl JP. The correlation between EDTA chelation
therapy and improvement in cardiovascular function: a meta-analysis. J
Adv Med. 1993;6:139-160.
13. Olszewer E, Carter JP. EDTA chelation therapy in chronic
degenerative disease. Med Hypotheses. 1988;27:41-49.
14. Olszewer E, Sabbag FC, Carter JP. A pilot double-blind study of
sodium-magnesium EDTA in peripheral vascular disease. J Natl Med
Assoc. 1990;82:173-174.
15. Rudolph CJ, McDonagh EW, Barber RK. A non-surgical approach to
obstructive carotid stenosis using EDTA chelation. J Adv Med.
1991;4:157-166.
16. Rudolph CJ, Samuels RT, McDonagh EW. Visual field evidence of
macular degeneration reversal using a combination of EDTA chelation
and multiple vitamin and trace mineral therapy. J Adv Med.
1994;7:203-212.
17. Casdorph HR. EDTA chelation therapy, II: efficacy in brain
disorders. J Holist Med. 1981;3:101-117.
18. Casdorph HR. EDTA chelation therapy: efficacy in arteriosclerotic
heart disease. J Holist Med. 1981;3:53-59.
19. Hancke C, Flytie K. Benefits of EDTA chelation therapy on
arteriosclerosis. J Adv Med. 1993;6:161-172.
20. Sloth-Nielsen J, Guldager B, Mouritzen C, et al. Arteriographic
findings in EDTA chelation therapy on peripheral arteriosclerosis. Am
J Surg. 1991;162:122-125.
21. Guldager B, Jelnes R, Jorgensen SJ, et al. EDTA treatment of
intermittent claudication – a double-blind, placebo-controlled study. J
Intern Med. 1992;231:261-267.
22. van Rij AM, Solomon C, Packer SGK, Hopkins WG. Chelation therapy
for intermittent claudication: a double-blind, randomized, controlled
trial. Circulation. 1994;90:1194-1199.
23. Schachter MB. Overview, historical background and current status
of EDTA chelation therapy for atherosclerosis. J Adv Med.
1996;9:159-177.
24. Gundy P. Cardiovascular diseases remain nation’s leading cause of
death. JAMA. 1992;267:335-336.
25. Winslow CM, Kosecoff JB, Chassin M, Kanouse DE, Brook RH. The
appropriateness of performing coronary artery bypass surgery. JAMA.
1988;260:505-509.