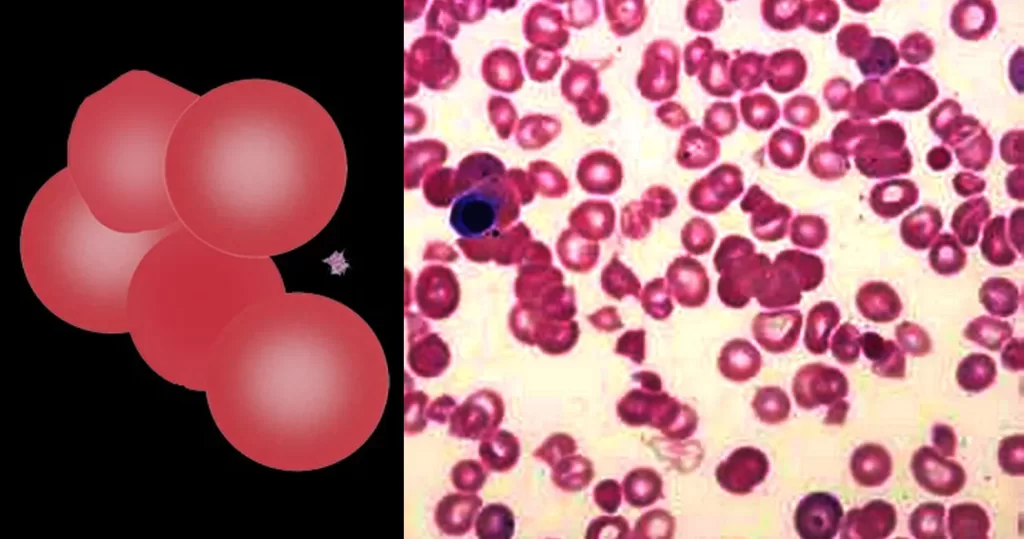
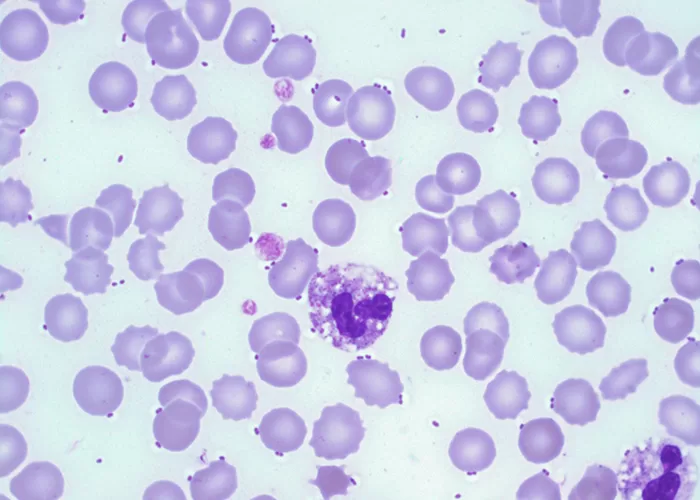
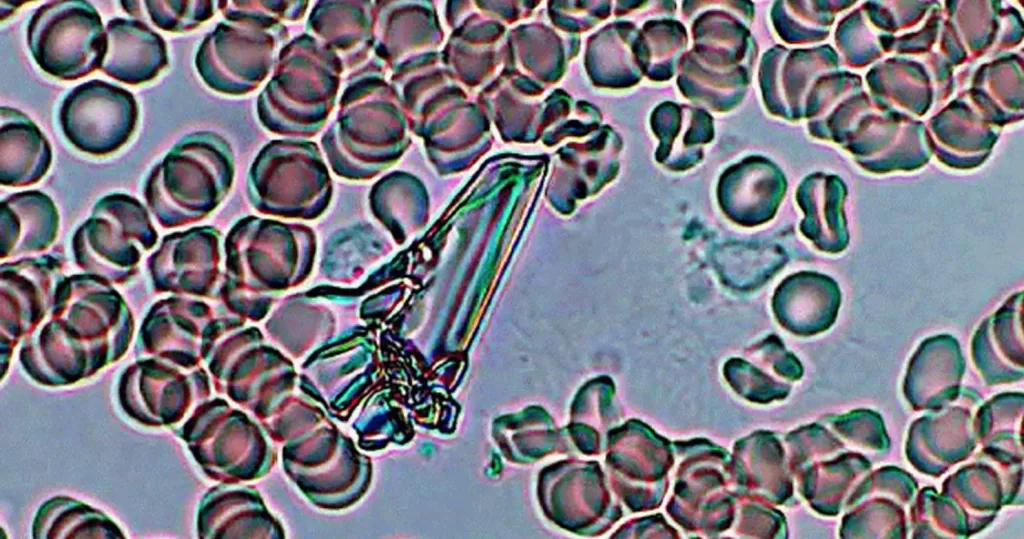
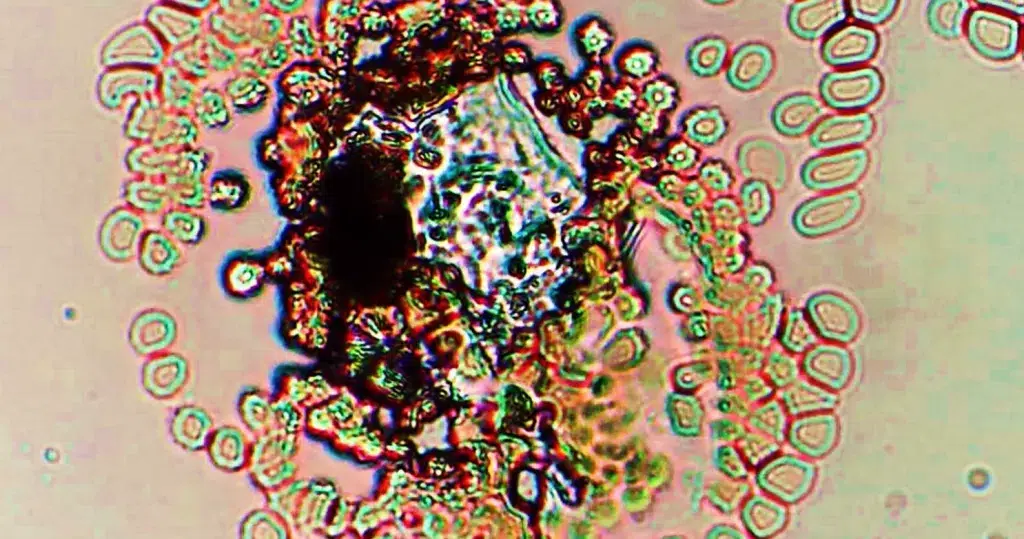
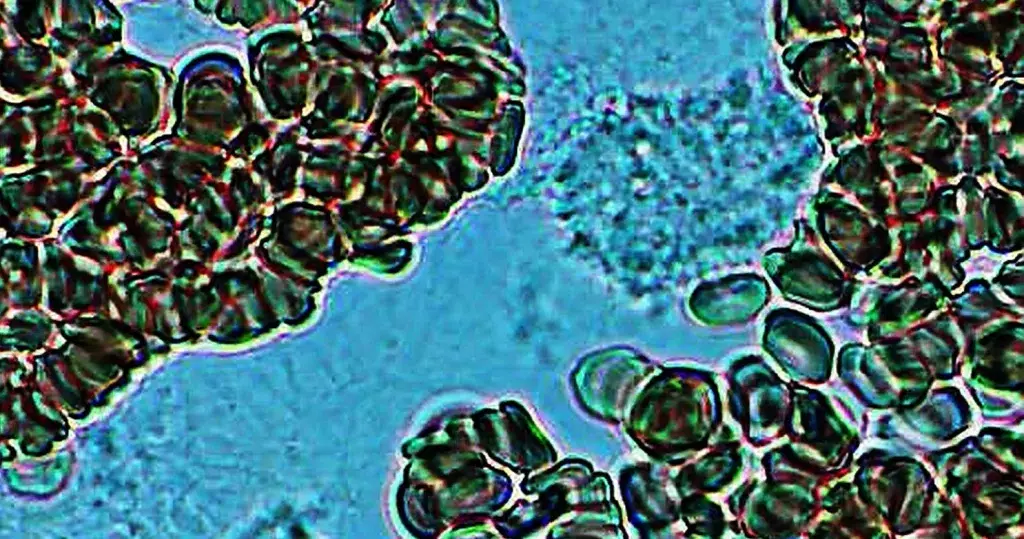
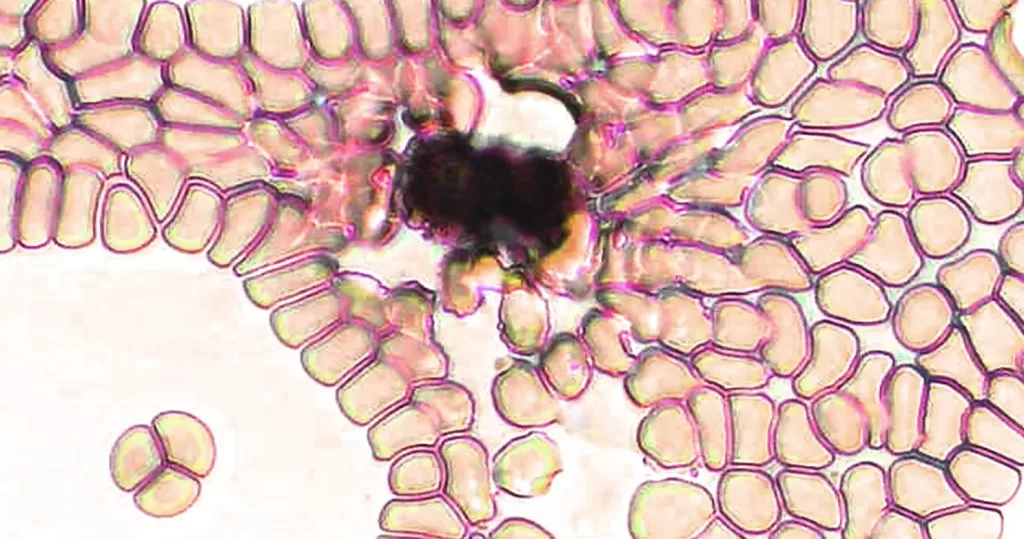
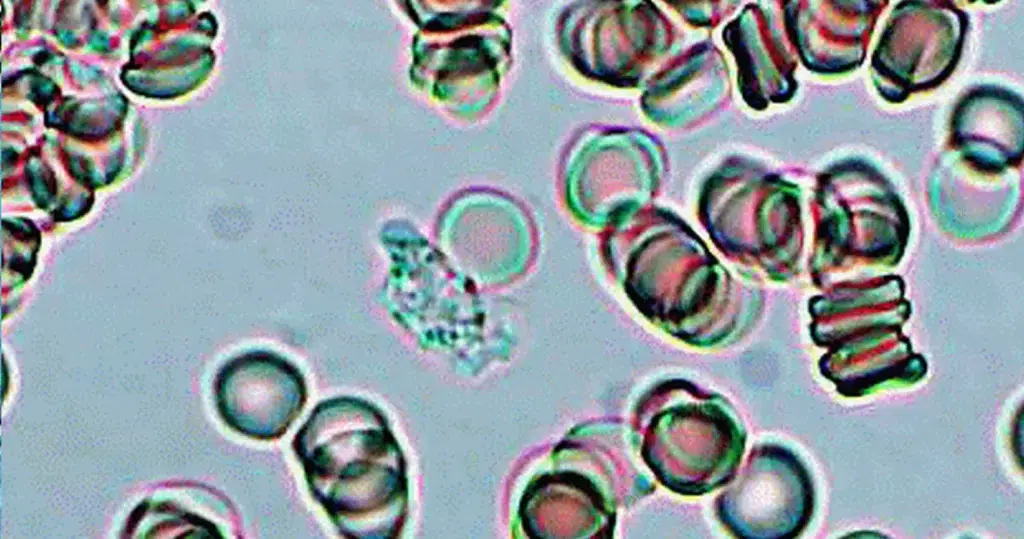
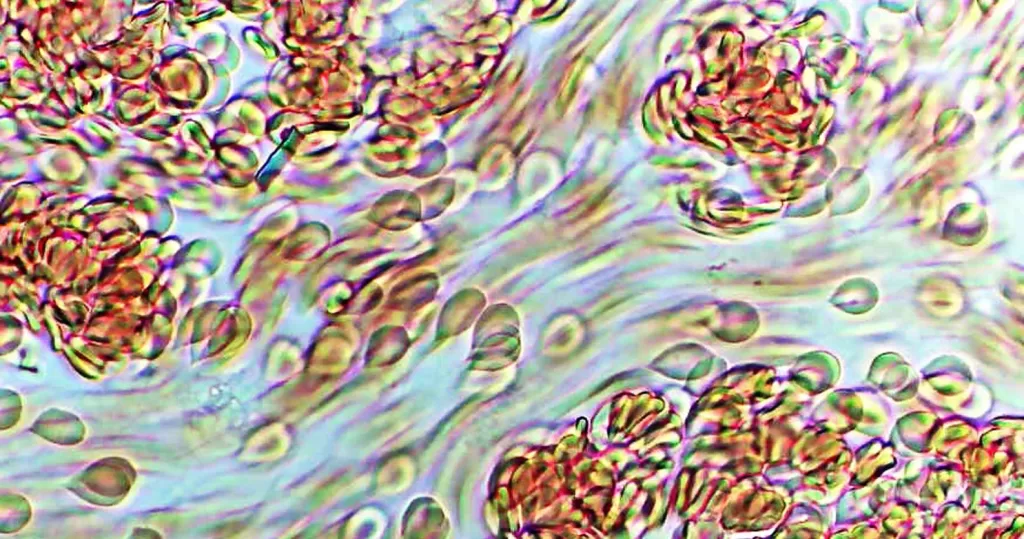
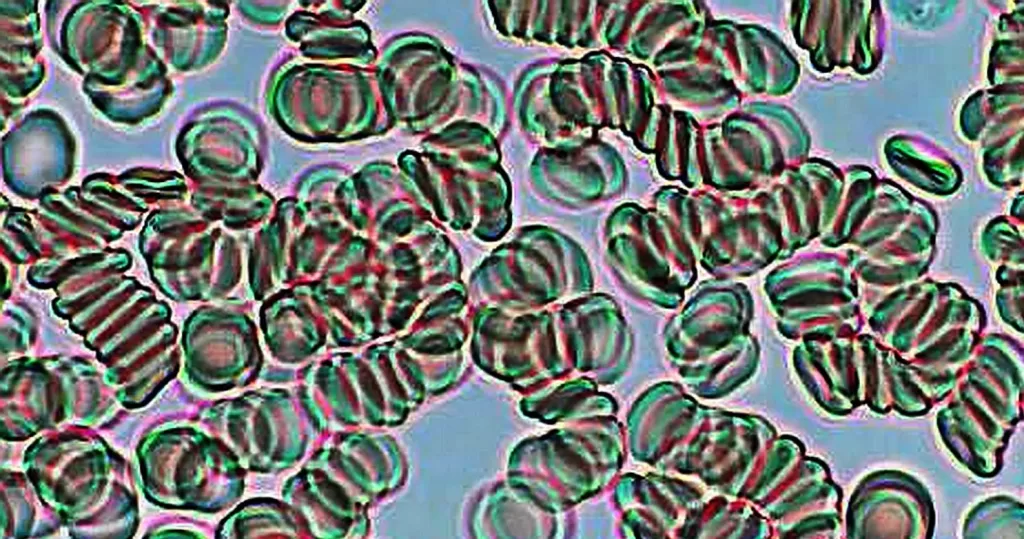
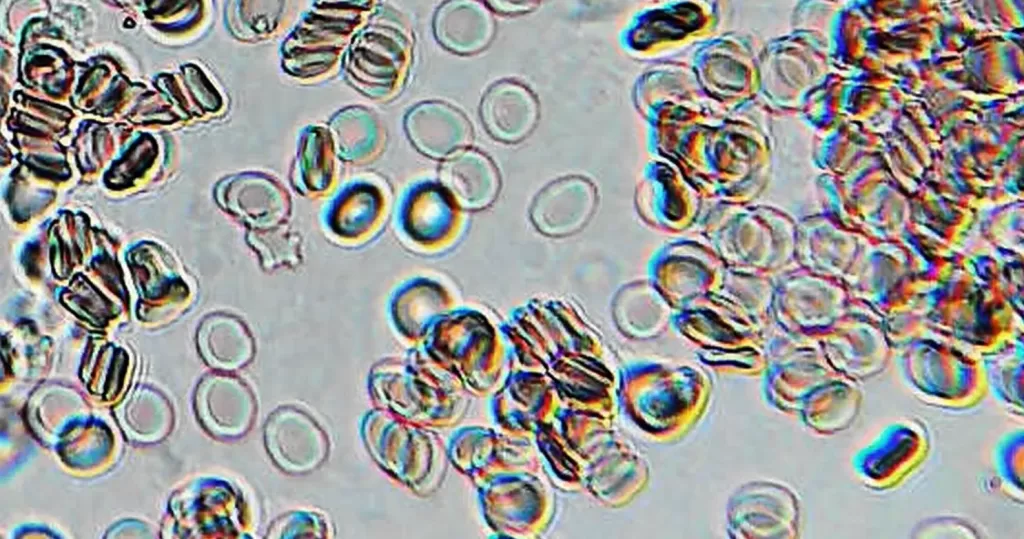
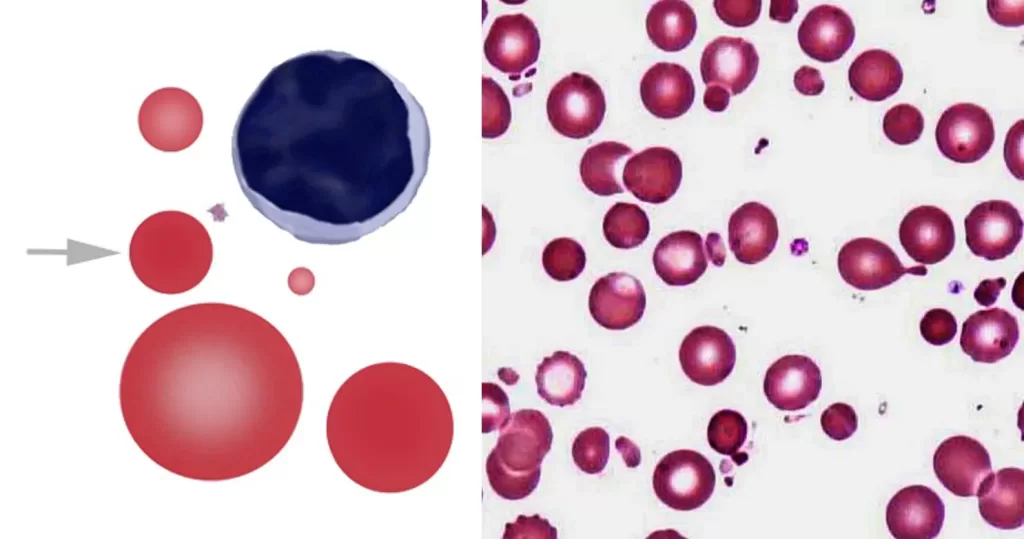
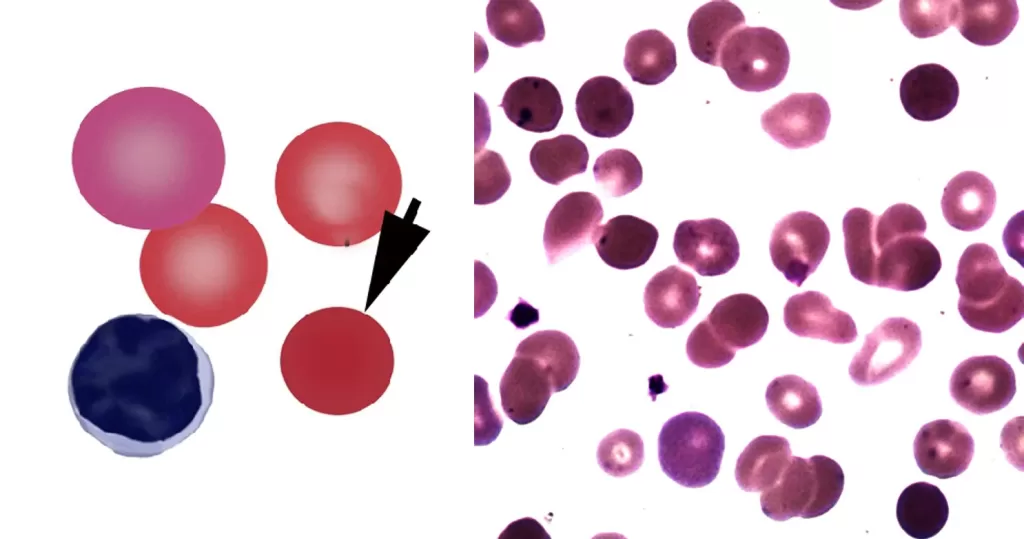
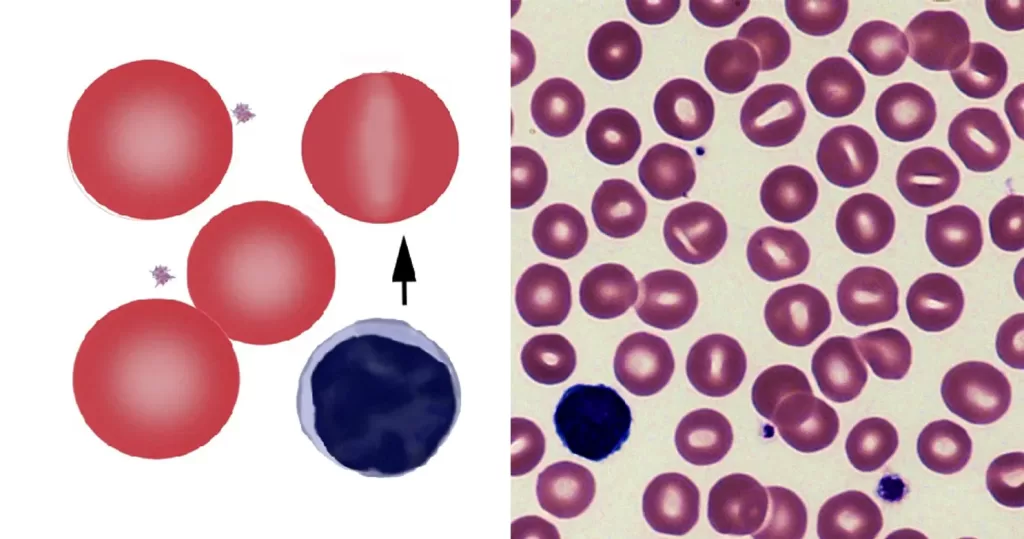
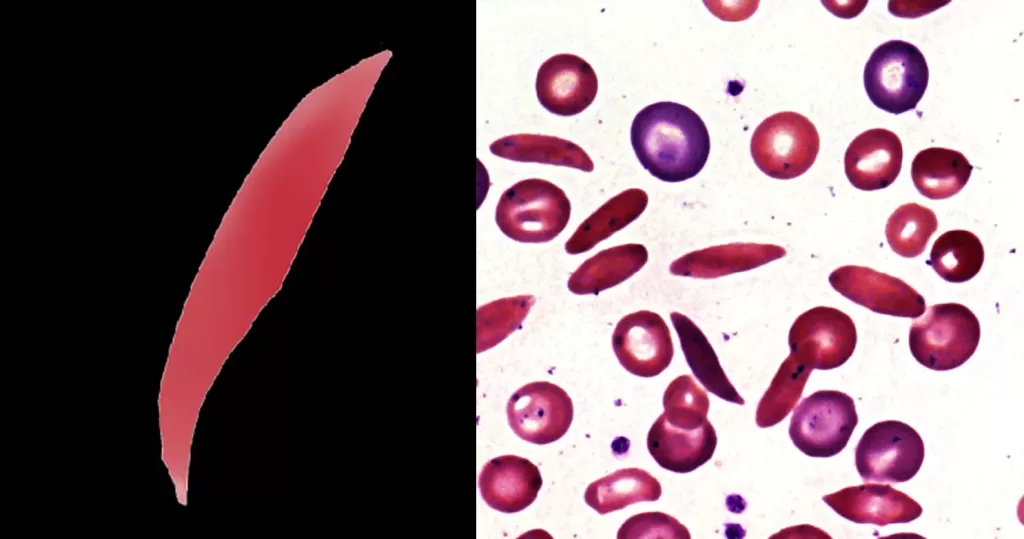
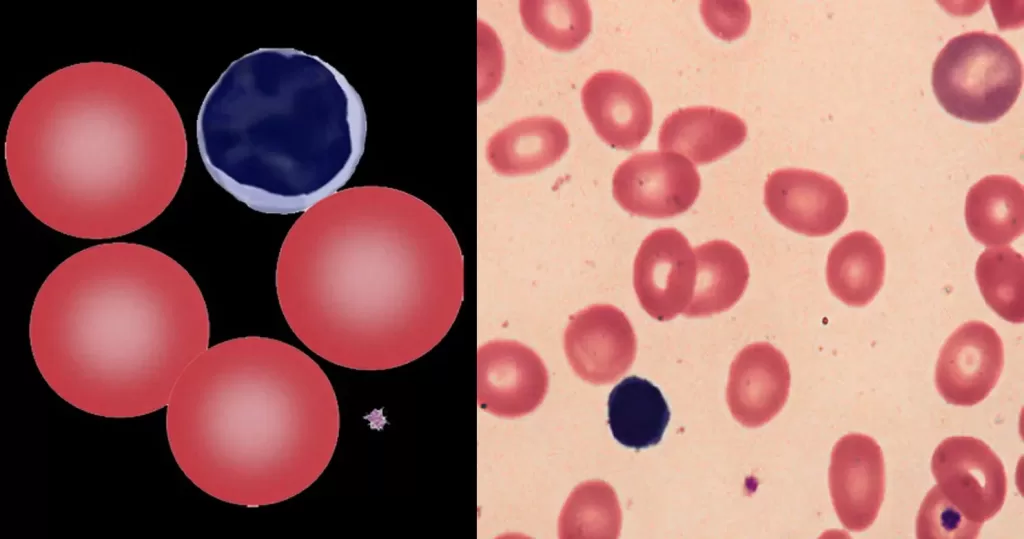
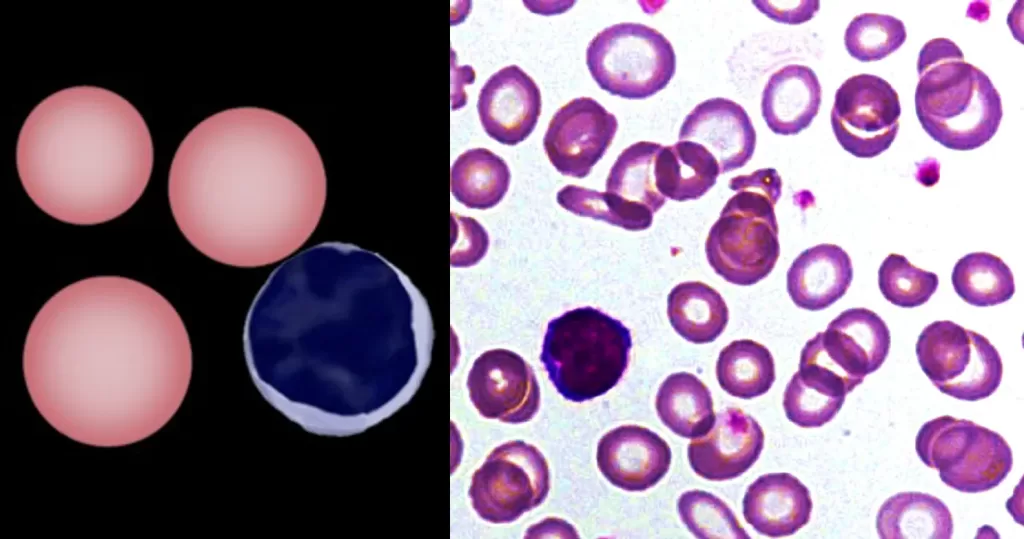
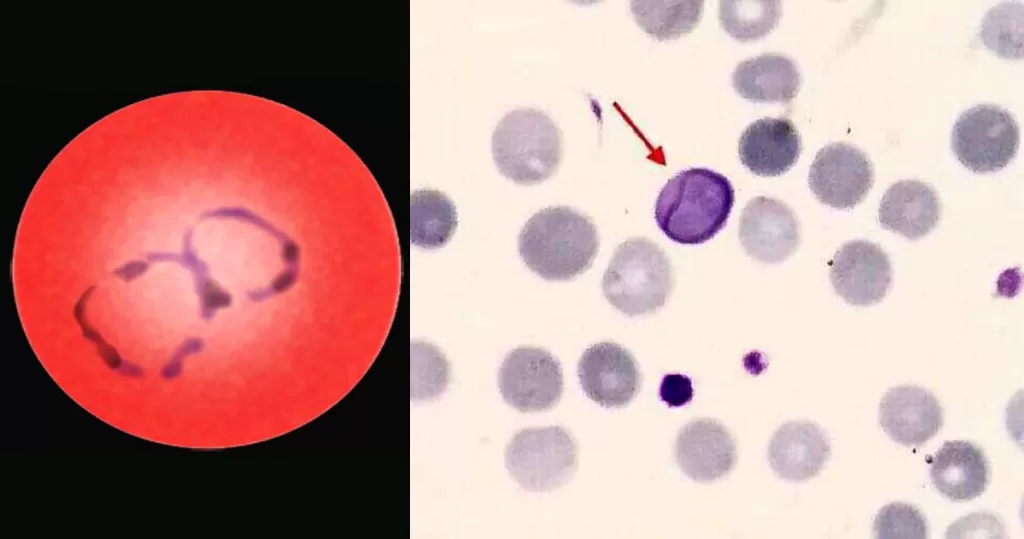
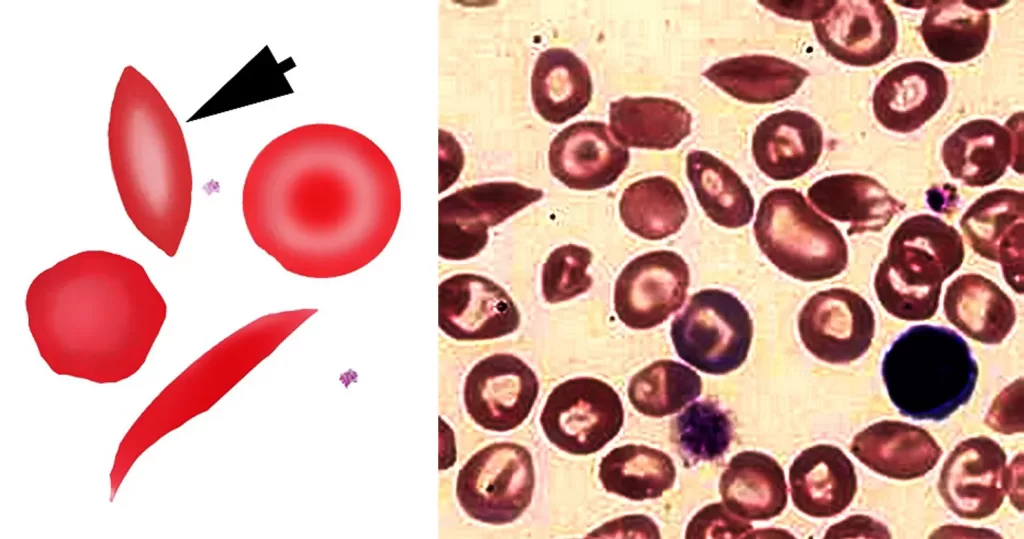
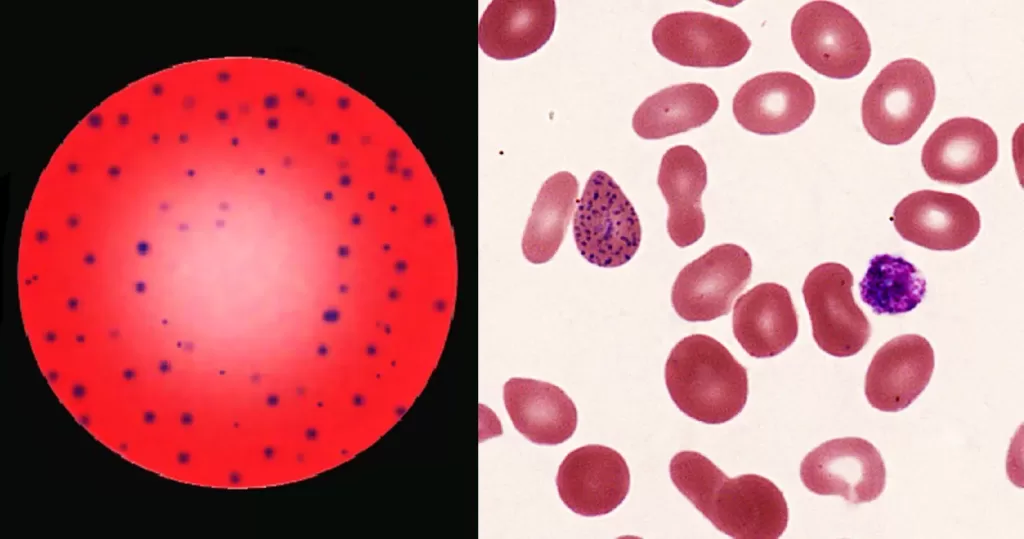
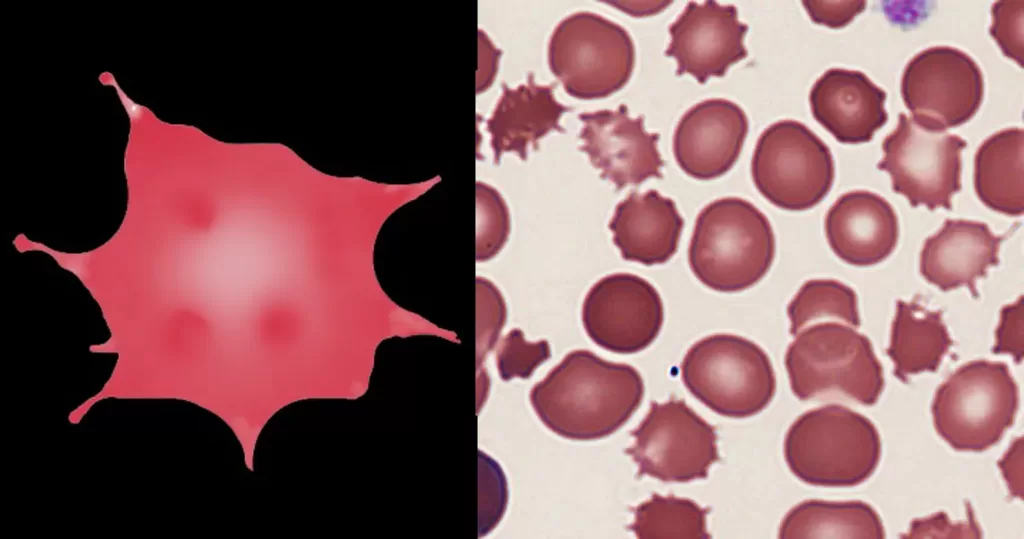
Agglutination
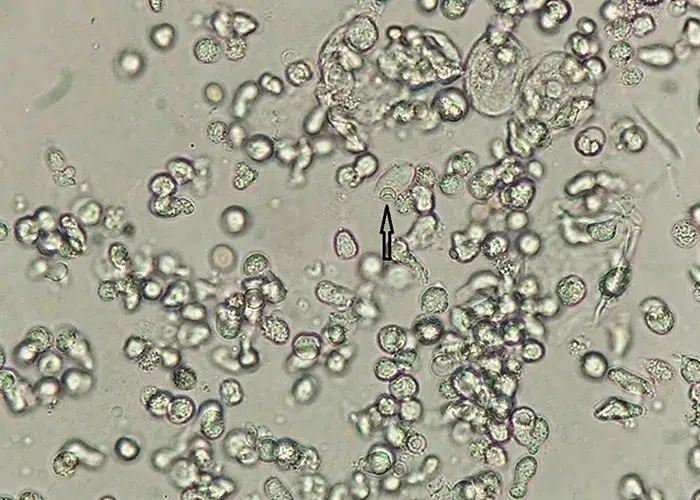
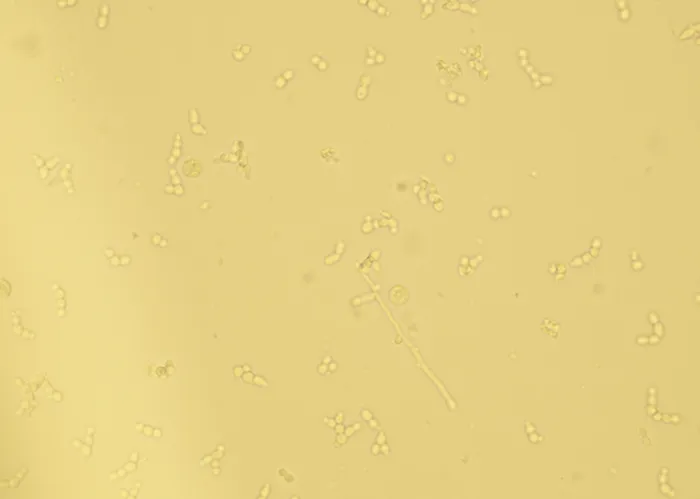
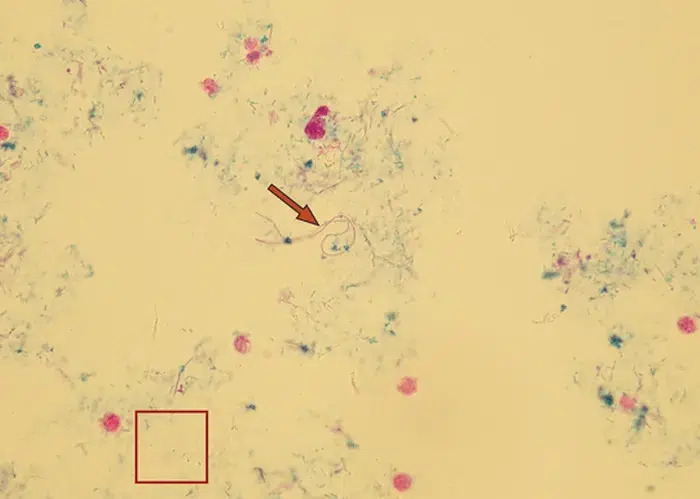
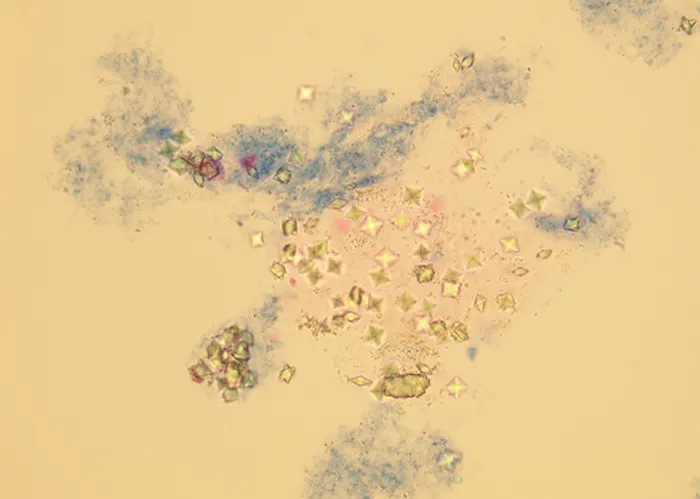
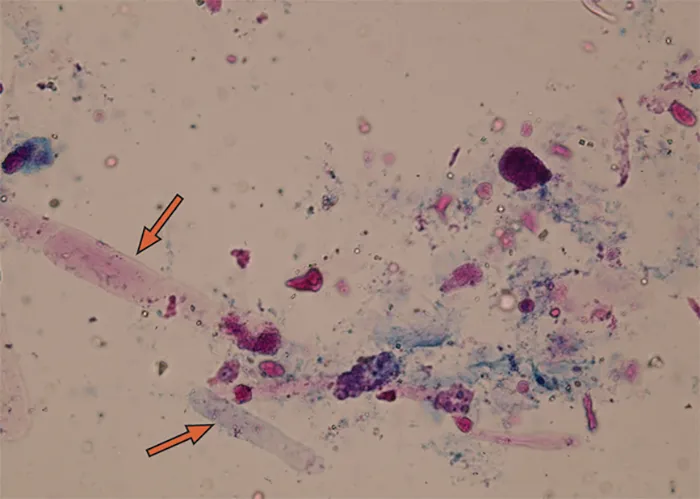
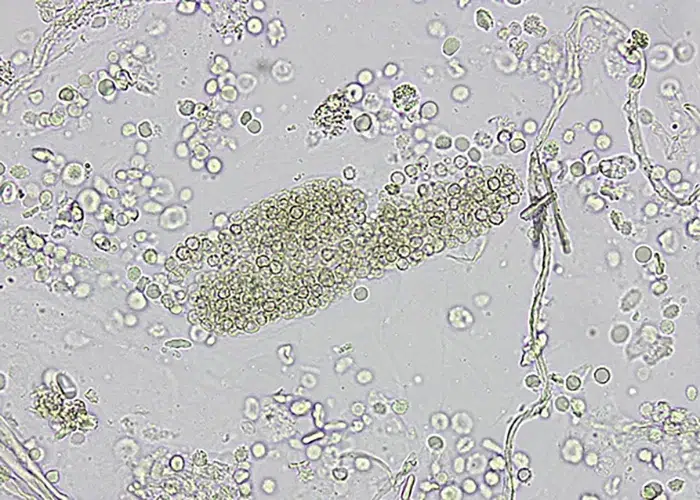
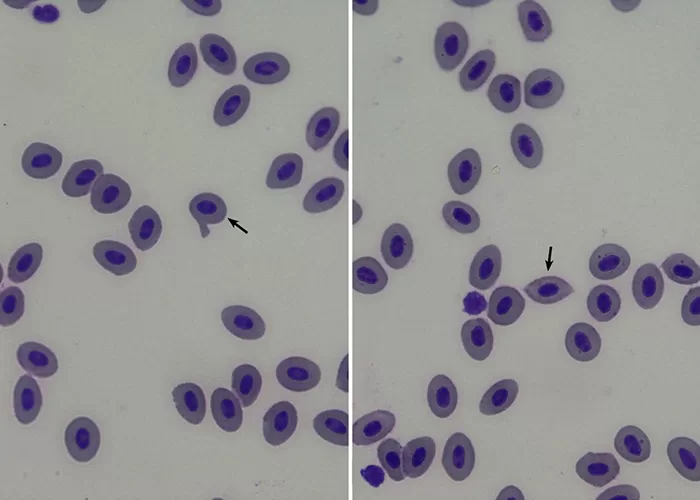
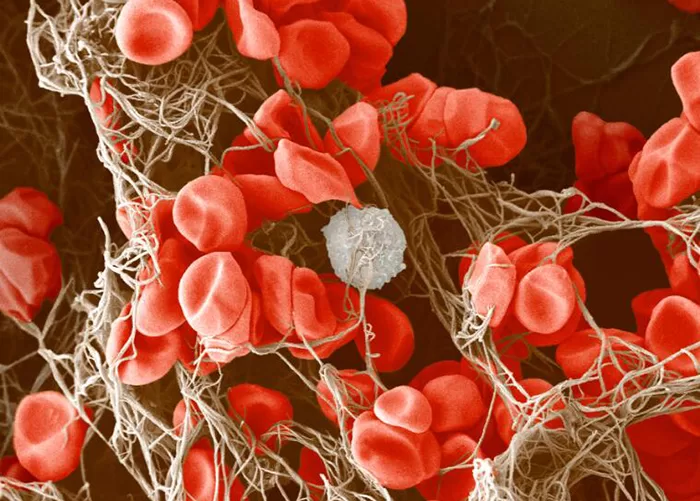
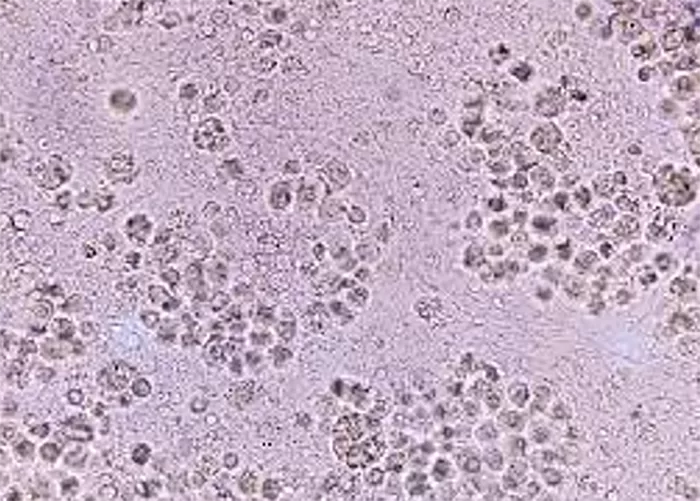
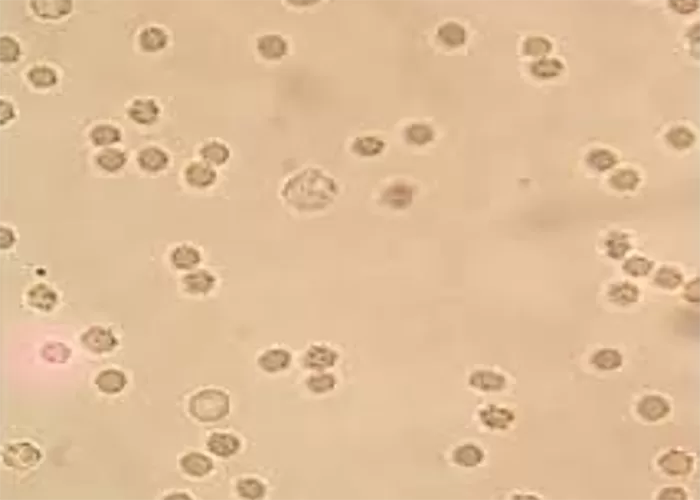
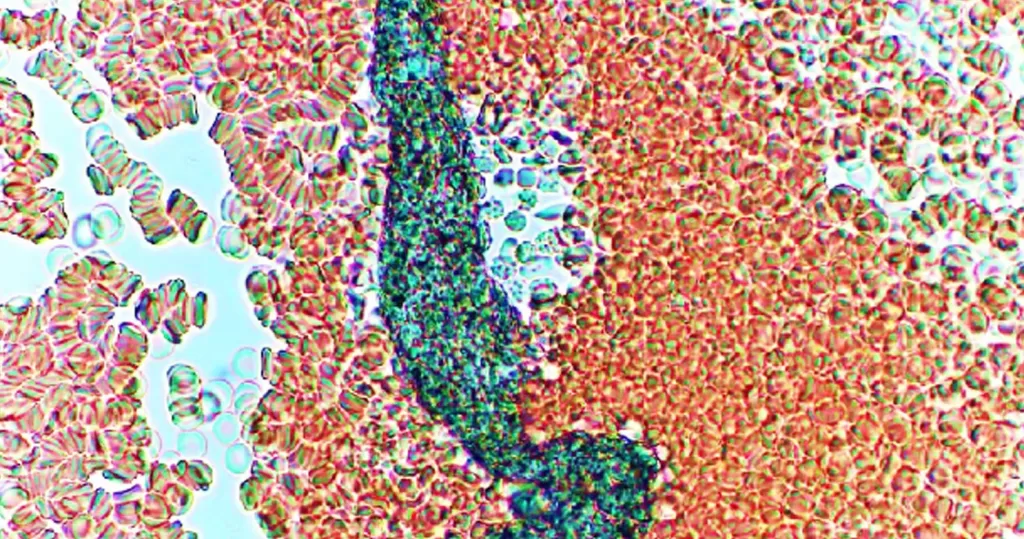
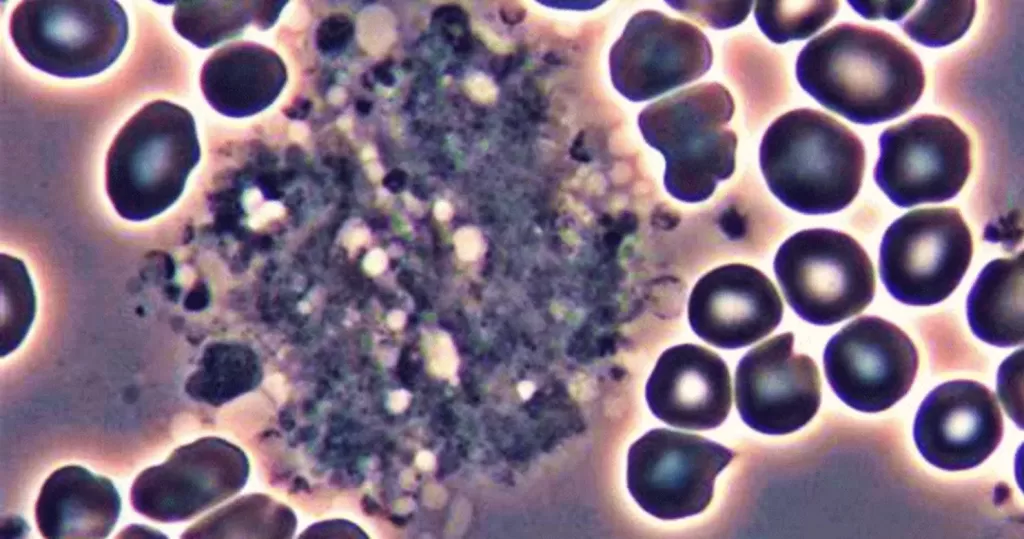
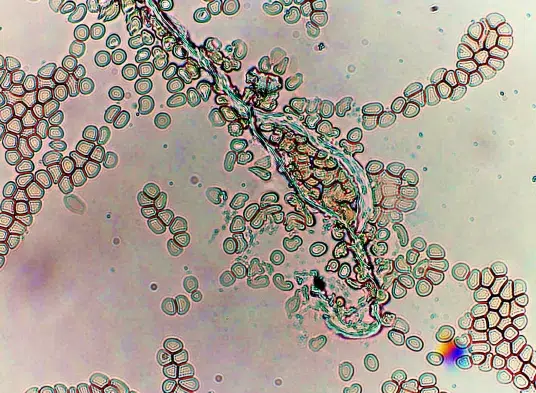
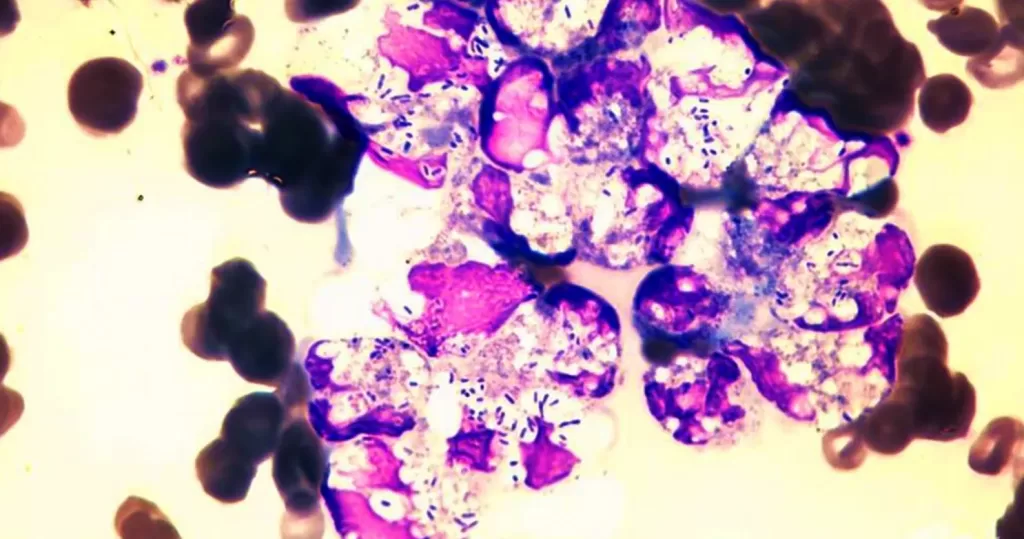
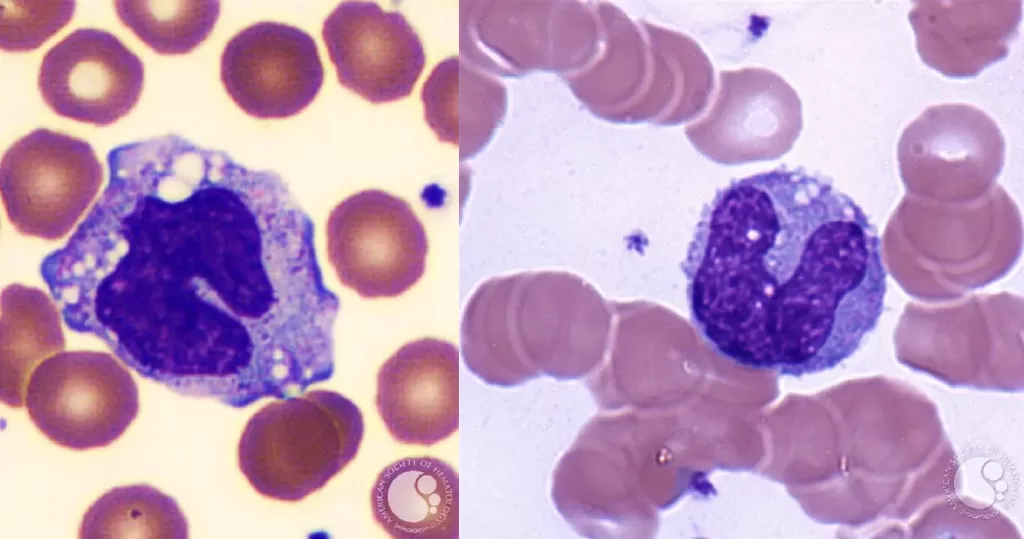
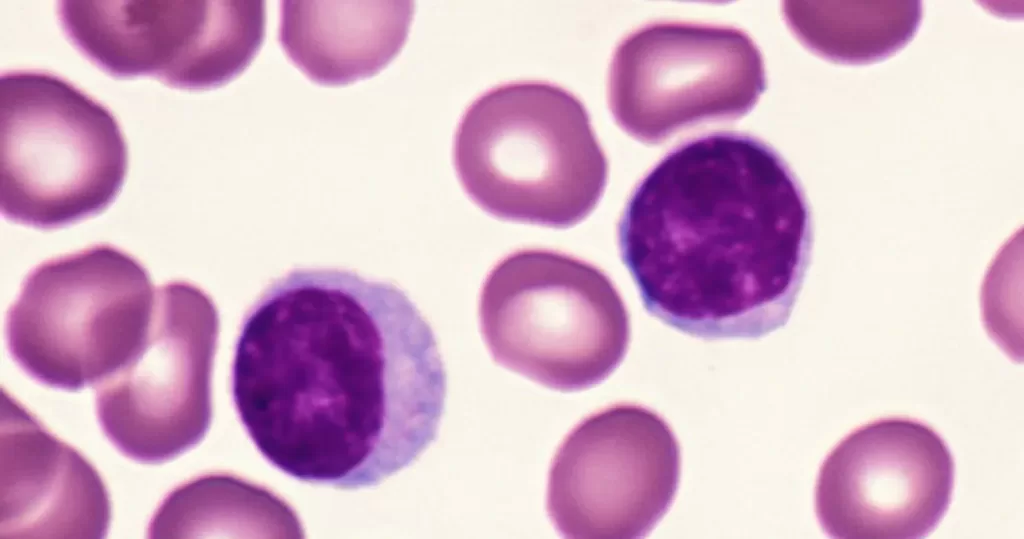
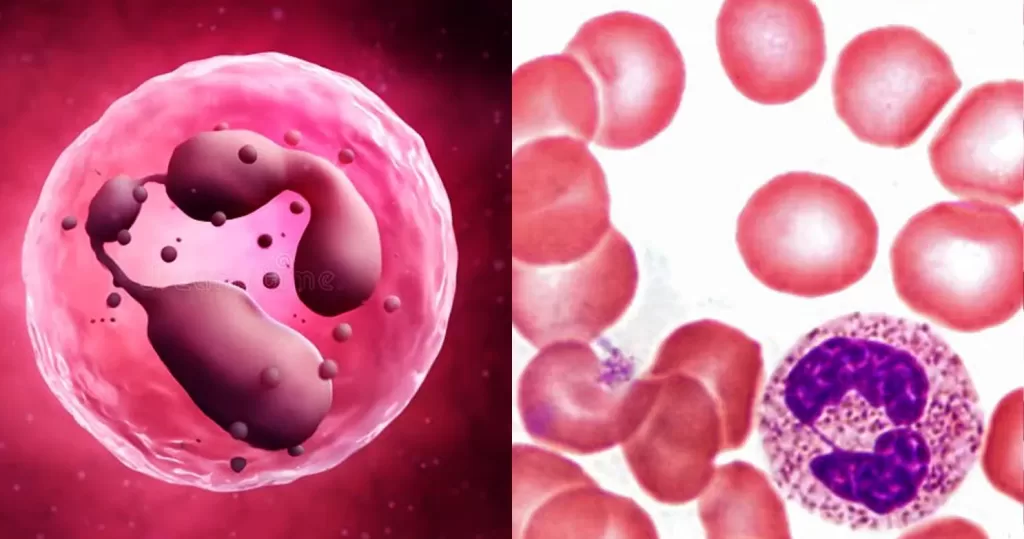
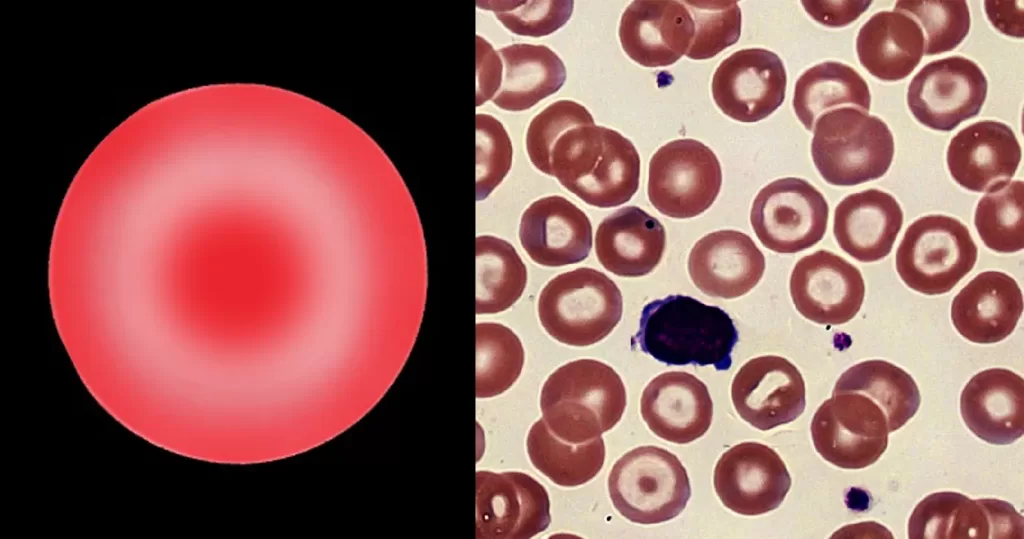
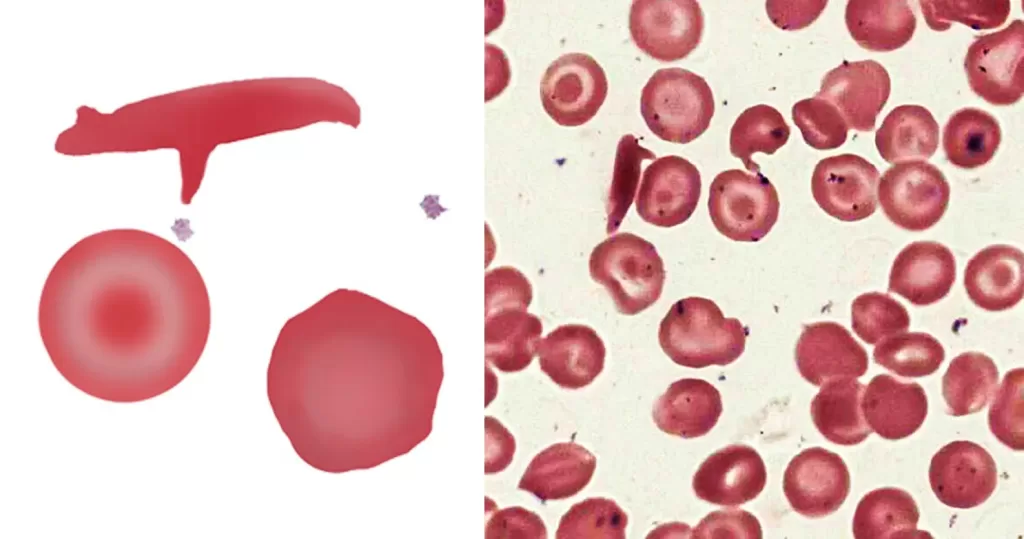
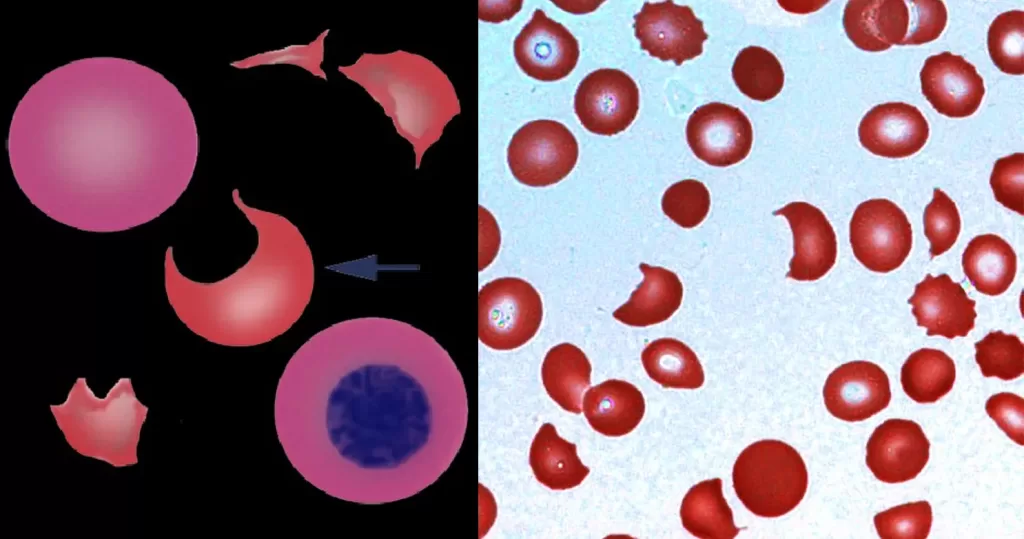
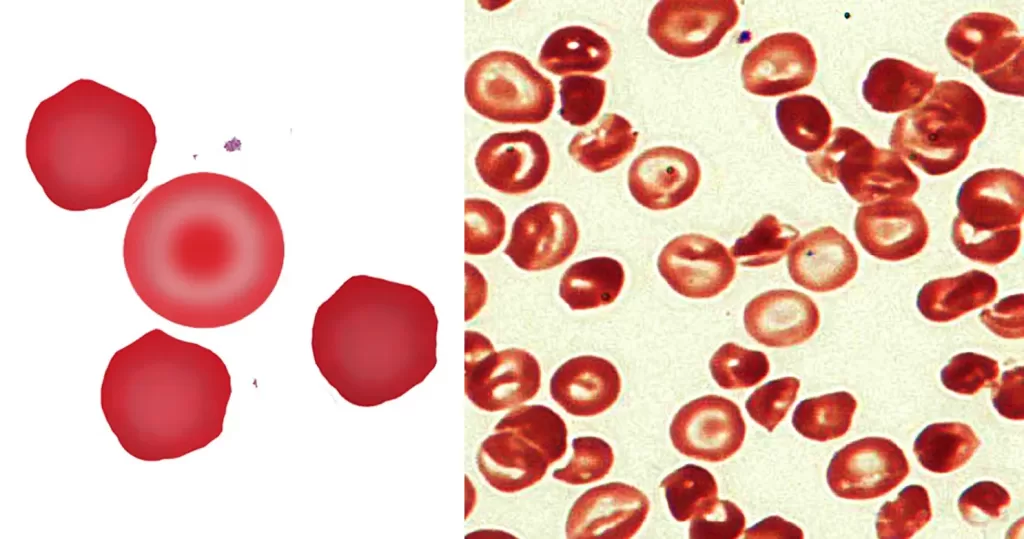
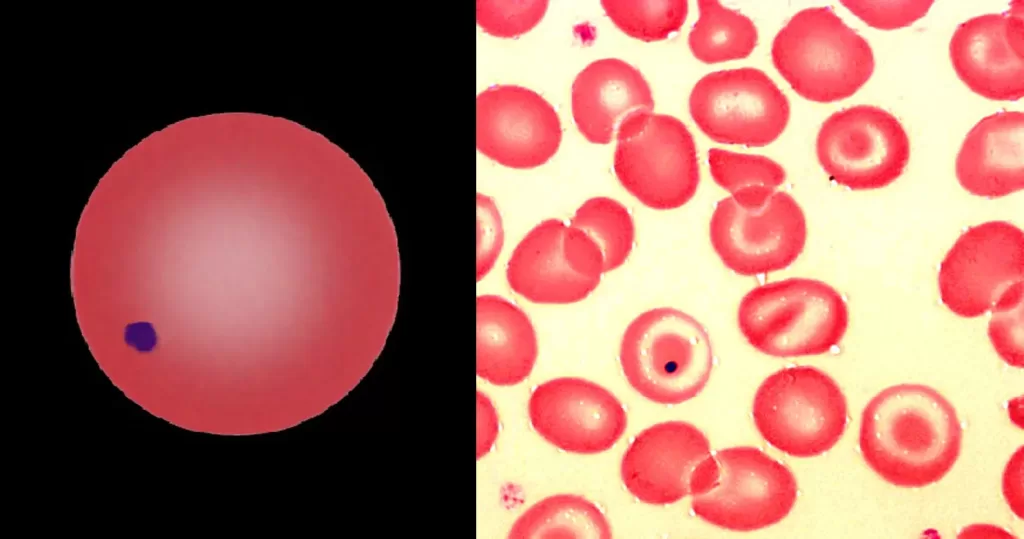
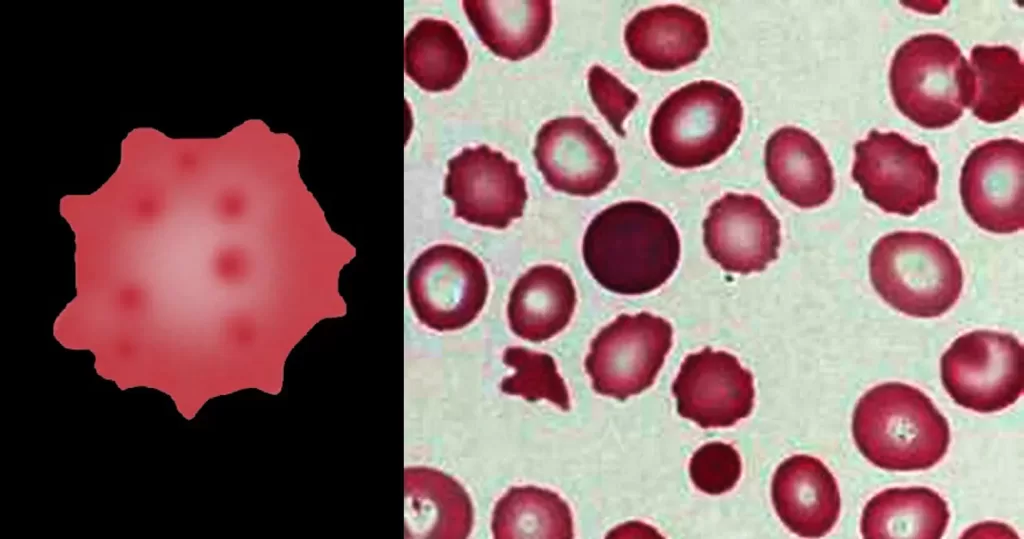
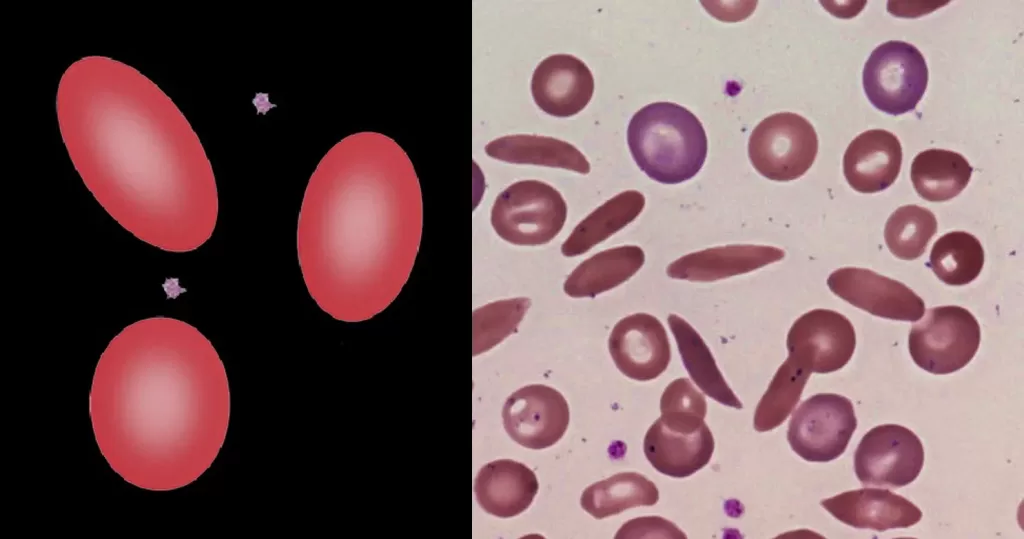
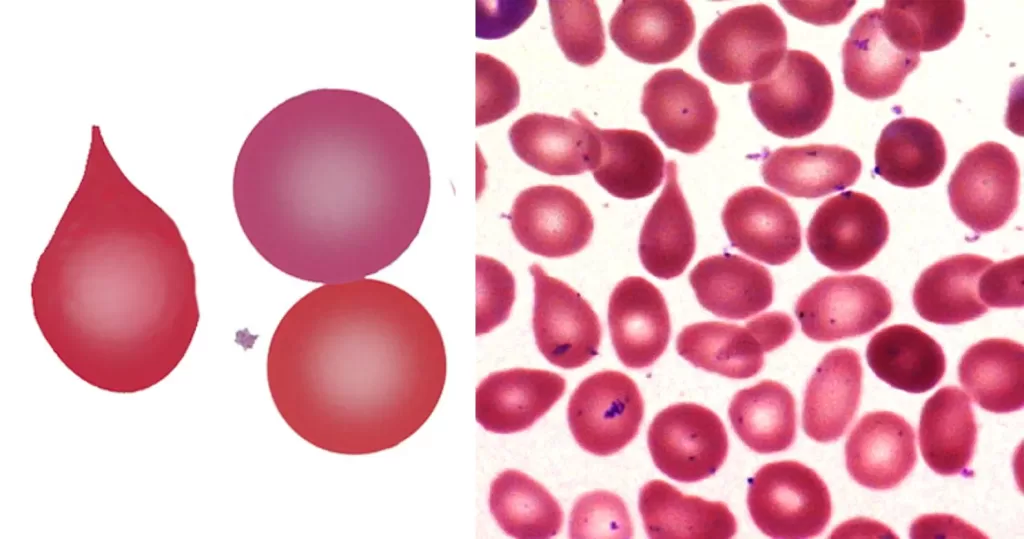
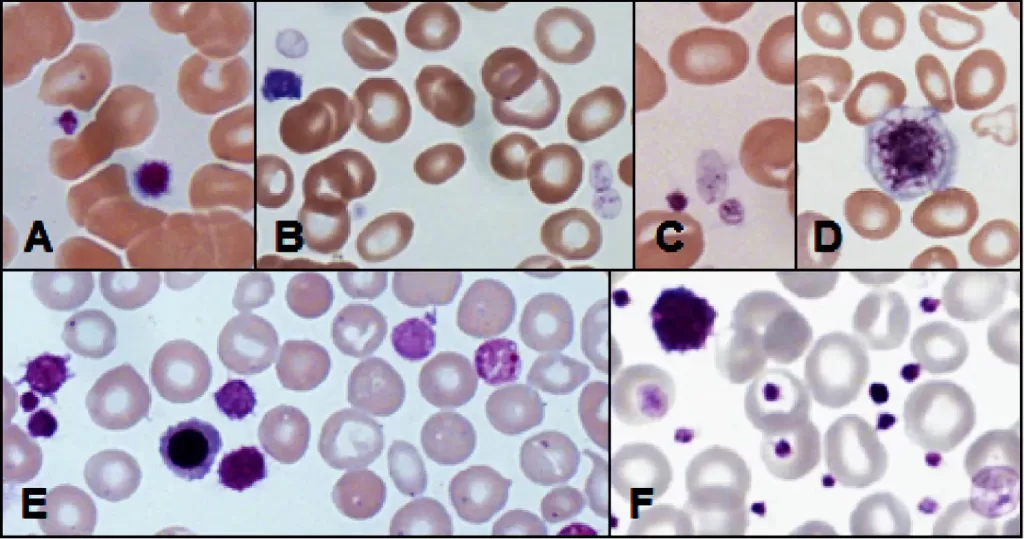
Agglutinates arise when antibodies attach to antigens on the membranes of adjacent red cells linking them together. The most common cause is “cold-reactive” IgM antibodies which do not cause overt symptoms. However, in some cases the effects may be clinically significant since antibodies may activate complement causing haemolysis, or the agglutinated cells can cause occlusion of small blood vessels in the cold (acrocyanosis). The clumped cells will sediment more rapidly leading to a raised erythrocyte sedimentation rate (ESR). Finally, the antibodies that cause cold agglutination may indicate an underlying malignancy (particularly lymphoma), or by acute infection.
https://haematologyetc.co.uk/index.php?title=Agglutination
Primary Causes:
- Monoclonal IgM frequently recognising blood group “I”, peak incidence in the elderly, but may arise from the 5th decade.
Secondary Causes (transient):
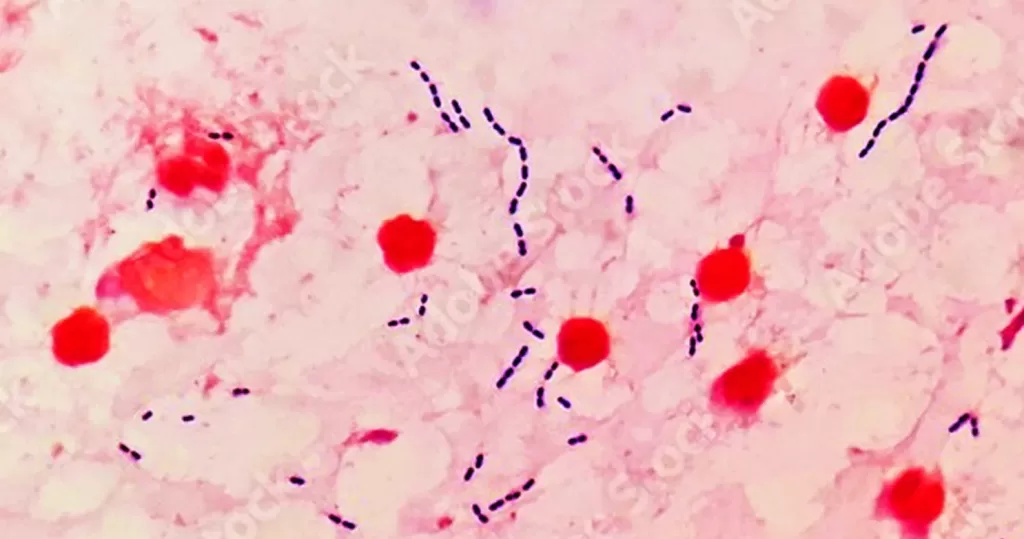
- Commonly: Mycoplasma pneumoniae or Epstein Barr virus
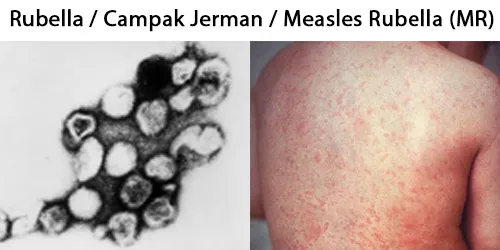
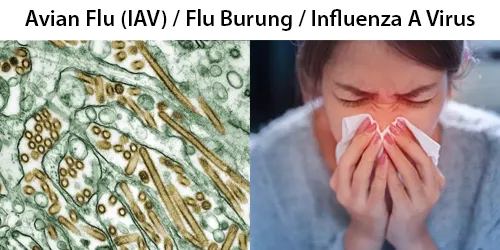
- Other viral including: influenza, HIV, CMV, rubella
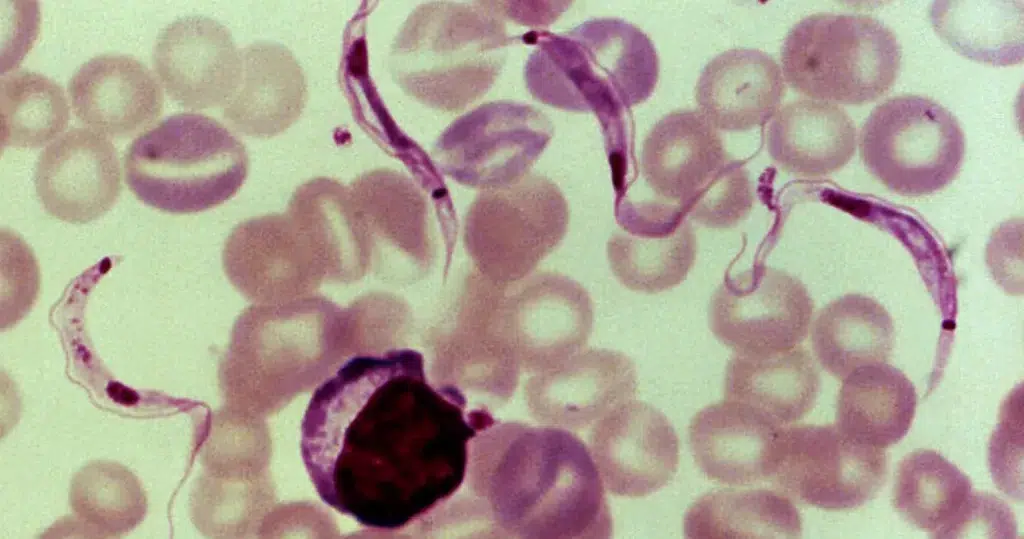
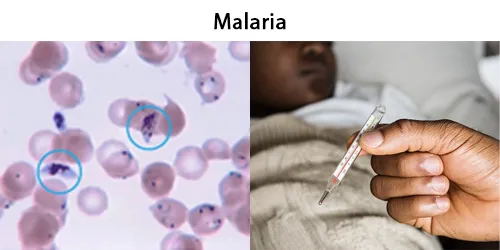
- Non-viral: bacterial endocarditis, syphilis, malaria
Secondary Causes (sustained):
- Commonly: Lymphoma, Waldenstroms macroglobulinaemia, CLL
- Rarely: Non-hematological malignancy
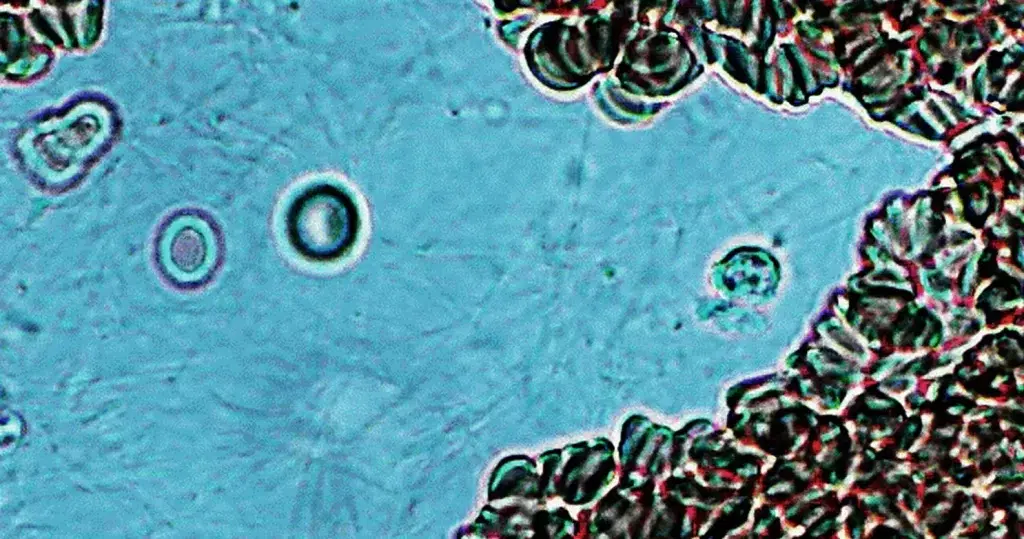
Donath Landsteiner antibody:
- Most commonly seen in chlidren, this IgG antibody recognises the P antigen – the clinical presentation differs: cold haemaglutinin disease (CHAD)
- Syphilis (congenital or tertiary syphilis classical but now uncommon)
- Viral: measles, mumps, influenza A, adenovirus, CMV, EBV and post-vaccination
- Bacterial: H.influenza, Mycoplasma pneumoniae Chronic idiopathic