Natural Health Techniques
Lab Test Result Meaning
What Do My Lab Test Results Mean? Blood and Urine Tests
Interpret your lab results here.
- LAB TEST RESULTS DISCUSSED:
- ALT (Alanine)
- Albumin/Globulin
- Alkaline Phosphatase (Alk Phos)
- AST (Aspartate aminotransferase)
- Bilirubin
- BUN (Blood Urea Nitrogen)
- C-Peptide
- Calcium
- Cholesterol (Total, HDL, LDL, VLDL)
- Creatinine (CK or CPK)
- GGT (Gamma glutamyltransferase)
- LDH (Lactate dehydrogenase)
- Phosphorus
- Potassium
- Sodium
- Total Protein
- Triglycerides
- Uric Acid
- Bile Acids
- CBC (Complete Blood Count)
- WBC (White Blood Count)
- Neutrophils
- Lymphocytes (including T and B cells)
- Monocytes
- Eosinophils
- Basophils
- Platelet Count (Thrombocyte count)
- RBC (Red Blood Cell Count)
- Hgb (Hemoblobin)
- HCT (Hematocrit or PCV or Pack Cell Volume)
- MCH (Mean Corpuscular Hemoglobin)
- MCHC (Mean Corpuscular Hemoglobin Content)
- RDW (Red cell Distribution Width)
- Blood Gasses (Oxygen, Carbon Dioxide, Bicarbonate)
- Cardiac Risk Factors
- Homocysteine
- Lipoprotein
- Thyroid Tests (TSH, Total and Free T3 & T4, Free Thyroxine
Index, T3 Resin Uptake, Thyroid Antibody test, Reverse T3, Cortisol
levels, Copper levels) - Diabetes and Blood Sugar tests (Glucose, Glycohemoglobin, IGF-1, Insulin, HOMA-IR)
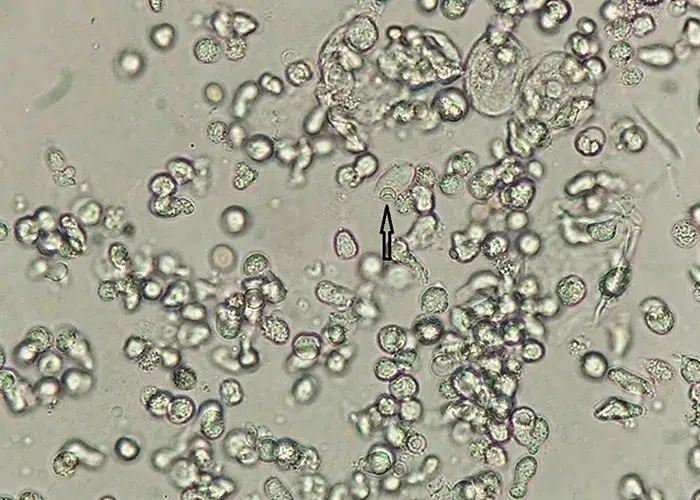
- Urinalysis (Volume, pH, Specific Gravity, Glucose, Protein, Blood, Bilirubin, Nitrate, Leukocytes and Sediment)
- Sex Hormone Profile Tests (Estrogen, Estradiol, Estriol, Progesterone, Testosterone)
- Tests for Sexually Transmitted Diseases (Herpes)
- FAQ?s about Lab Work
Blood Lab Test Results (Bloods for short):
Reference ?normal? ranges and unit measurements can vary from lab to
lab (sometimes up to 30% difference). Other factors influencing test
results include, dietetic preferences, sex, age, race, species,
menstrual cycles, amount of exercise, use of non-prescription drugs
(aspirin, cold medications, vitamins, etc.), prescription drugs, alcohol
consumption, collection and handling of the specimen. For best
comparisons of lab results, tests should be done in the same lab. Always use the normal ranges printed on the lab test result report of that particular sample.
Blood tests can have false positives and negatives. Interpretation of
blood tests takes knowledge of the underlying disease process and
experience. If your lab results are outside the normal range, we suggest
that you discuss them with your doctor. Often it is not the recent
result, but the change from a previous test that is most helpful in
trying to place a diagnosis on a condition.
Some tests cost more than others. If you can help the doctor
understand why a certain test may be important for you and they can
justify it in their mind, you may get to your diagnosis quicker and your
insurance may pay for the test saving time, money, and aggravation.
When a doctor evaluates the results of a lab test, they try to figure out what all the causes could be then ?rule out?
the ones that don?t seem to fit after you add all the other signs and
symptoms into the picture. This is much like putting a jigsaw puzzle
together and searching for the exact placement of the pieces to the
puzzle. This Sherlock Holmes activity is one of my favorites because I
get to add in so many other tidbits of information that the medical
system doesn?t have time to ask in making a final ?jigsaw puzzle?
assessment. Below are lists of ?Rule Outs? for
both high and low levels. You will see a veterinary flare to these as I
have put in the rule outs for animals as well. I have included the
medical term under each abnormality in parentheses. I have also tried to
explain in laymans terms the meaning of many of the scientific jargon.
To read more about Rule Out?s and what this term means, go to: http://naturalhealthtechniques.com/BasicsofHealth/what_is_a_rule_out.htm
The Basic Blood Chemistry Panel (Also called a Panel, Serum Chemistry Panel, Chemistry Screen, BMP or Basic Metabolic Panel):
For these lab tests, blood is drawn from the patient who has been
fasting 12 hours or more. Three tubes of blood are usually drawn from a
vein in the arm (human) or neck (animals).
________________________
Alanine (ALT, Alanine aminotransferase?formerly known as SGPT).
ALT is an enzyme contained inside the fluid part of each liver cell.
The larger the number of cells that are damaged, the higher the number.
This lab test is a good indicator of acute disease (disease coming on
quickly), but not for chronic liver diseases like cirrhosis where the
cells have died and been replaced by fibrous tissue. ALT stays in the
blood stream for about 60 hours. Because of this, sometimes your doctor
will want to repeat the blood lab test to track how the body is
responding.
ALT Too High (Liver enzymes elevated): Rule out
hepatocellular (liver cell) diseases such as cancer, fatty liver, cell
death due to bacteria/viruses/hepatitis or toxins, cirrhosis,
obstructive jaundice, and infectious mononucleosis.
ALT Too Low: Rule out pyridoxine (Vitamin B6) deficiency.
Albumin and Globulin
-This lab test measures the amount and type of
protein in your blood. Albumin and globulin are a general index of
overall health and nutrition. Globulin is the ?antibody? protein
important for fighting disease produced by white blood cells. Albumin
contains things like clotting factors, fibrin and binding proteins (much
like egg white) and it give the blood more substance.
Albumin/Globulin Too High: Rule out dehydration,
diabetes insipidus (low blood sugar diabetics that can?t get enough
water), antigenic responses, infection, and gammopathies such as
lymphosarcoma, multiple myeloma, and FIP?Feline Infectious Peritonitis
Albumin/Globulin Too Low: Rule out malnutrition,
overhydration, advanced liver disease, cancer, acute or chronic
hemorrhage, kidney disease (nephrosis), burns, multiple myeloma,
metastatic carcinomas, heart disease, loss of blood or protein into the
body cavity, malabsorption, parasites and pancreatic atrophy.
False Positives: False elevations in this lab test
can occur with red blood cell damage in the sample (hemolysis) and
lipemia (fat in the blood).
Alkaline Phosphatase (Alk. Phos.)
Alkaline phosphatase is an enzyme found primarily in bones and the
liver but can also be found in other tissues of the body as well such as
the intestine, kidney, placenta and in white blood cells. It is thought
that this enzyme is increased in the body only when there are actively
growing new cells being produced. Alkaline Phosphatase enzymes can be
further broken down to find out where they are specifically being
produced using a process called electrophoresis (a
special test not included in the regular blood panel). The alkaline
phosphatase enzyme circulates in the body for about three days before it
starts to break down, so if your blood tests are repeatedly high in
this area, there are actively growing cells.
Alkaline Phosphatase Too High: Rule outs include
gallstones, damage to bones, Paget?s disease (a chronic disorder of the
adult skeleton in which localized areas of hyperactive bone are replaced
by a softened and enlarged osseous structure), rickets, healing
fracture, hyperparathyroidism, pulmonary infarction, heart failure,
liver disease with too many cells growing (like cancer), obstruction
within the liver or the liver not getting what it needs because
something is obstructed outside the liver, pancreatitis, severe anemia,
lack of oxygen getting to the liver, Cushing?s disease, drugs such as
glucocorticoids (steroids), primidone, phenobarbital (anti-seizure
drugs). An elevated alkaline phosphatase is normal in growing
children and in pregnant women.
Alkaline Phosphatase Too Low: Pernicious anemia,
hypoparathyroidism, hypophosphatasia and possibly the blood was taken
from a collection tube that had EDTA preservative in it.
AST (Aspartate aminotransferase?formerly known as SGOT):
AST is an enzyme contained in all cells of the body, but is used as a
diagnostic marker for liver and muscle damage. Its half-life is about
12 hours.
AST Too High: Rule out liver disease (death of cells
and cancer), skeletal muscle diseases, (myositis and muscular
dystrophy), trauma, pancreatitis, renal infarct, eclampsia (milk fever),
cancer, cerebral damage, seizures, alcohol, heart tissue disease (heart
attacks, pericarditis), infections in the bloodstream (septicemia),
intramuscular injections, drugs such as corticosteroids, primidone,
antibiotics and other drugs processed through the liver. Hemolysis
(ruptured red cells from improper handling of the blood) can also raise
AST levels.
AST Too Low: Rule out pyridoxine (Vitamin B6) deficiency, and terminal stages of liver disease.
Bilirubin (Bilirubinemia):
Most bilirubin (80%) is a breakdown component from dying red blood
cells. Bilirubin is also in macrophages of the spleen and in the liver,
bone marrow and non-heme porphyrins. Bilirubin travels via the blood
stream in the plasma part of the blood surrounded by albumin, globulin
and other proteins. As it gets to the liver via the blood system, it
disassociates from these proteins and the liver accepts it into it?s own
cells by binding (conjugating) it with glucuronic acid. This
conjugation makes it water-soluble. From here bilirubin gets into the
bile and then dumps into the small intestine, eventually leaving though
the feces after it changes form one more times. Some of this bilirubin
sneaks back into the bloodstream and is reabsorbed into the blood. This
happens repeatedly. Sometimes the bilirubin ends up being excreted via
the kidneys and dumps out into the urine. When this happens, it shows up
in abnormal levels within the blood and may also show up in the
urinalysis lab test on the dipstick test.
Bilirubin lab test Too High (Hyperbilirubinemia):
Rule outs include hemolytic anemia, pulmonary infarct, Gilbert?s
syndrome (mild unconjugated hyperbilirubinemia), Dublin-Johnson syndrome
(a genetic symptomatic mild jaundice), neonatal jaundice, inadequate
liver uptake or defective conjugation, massive internal hemorrhage,
obstruction of bile within the liver or outside the liver, defective
secretion, acute or chronic hepatitis, fibrosis of the liver and liver
cancer. It can also be falsely elevated when there is too much fat in
the bloodstream. If only slightly elevated above the expected ranges,
but with all other enzymes (LDH, GOT, GPT, GGT) within expected values,
it is probably a condition known as Gilbert?s syndrome and is not
significant.
Bilirubin is also measured in the urine. Sometimes
the doctor?s will run a test to check both conjugated and unconjugated
bilirubin to help them determine where the extra is coming from.
They want to know if the liver is blocked or the blood cells have
broken (hemorrhage). When the liver is blocked totally the fecal
material will also be gray or whitish (acholic). When increased
bilirubin is caused from hemorrhage the stools will be almost orange in
color. You will want to tell your doctor this information because they
may not ask.
Bilirubin lab test Too Low: Low values are of
no concern. Sunlight and fluorescent lights degrade the sample as the
bilirubin is very fragile when exposed to light.
BUN (Blood Urea Nitrogen, Urea Nitrogen):
High BUN values in the lab tests may mean that the
kidneys are not working as well as they should in clearing out the
breakdown products of digested protein. The major breakdown product of
protein you eat is urea, which is first formed in the liver. Urea
contains nitrogen and together, in excess quantity, they are both toxic
to the body and must be removed. Kidneys normally do an excellent job of
removing urea, but when they start to fail, the urine components get
all backed up in the system and the blood concentration of urea begins
to rise. If you smell the breath, it has a stale, sickly smell (see my
handout on the causes of Halitosis for other characteristics of bad breath: http://naturalhealthtechniques.com/specificdiseasesbad_breath_causes_%20and_%20remedies.htm ) The reference range (or range within which most normal people?s test values fall) for BUN is 10-20 mg/dl.
BUN lab test Too High (Uremia, Azotemia or Uremic Acidosis):
Rule out dehydration (too little water in the tissues), too much
exercise, shock due to too much blood being lost (hemorrhagic shock),
pancreatitis, intestinal foreign body, adrenal cortical insufficiency
(adrenal glands not producing enough of the hormones it is suppose to be
producing), or any condition which decreases blood flow to the kidneys,
glomerulonephritis (the little tubules that make the urine in the
kidneys are swollen and not working right), amyloidosis (the kidney
tissue is being replaced with some kind of unnatural protein),
pyelonephritis (inflammation/infection of the kidney where the urine
pools before it dumps out into the ureters), nephrosis (a condition of
the kidneys), calcium nephropathy?also called lymphosarcoma (cancer of
the kidneys where the tissues are being replaced by calcium so the urine
can?t get out), kidney cancers, obstruction of the urine coming out of
the kidney, leukemia, heart failure, ruptures of the urine carrying
parts (kidney, ureters, bladder, urethra, kidney tubules), too much
protein in the diet, bleeding within the intestine, and drugs like
amphotericin B. Often, an additional test is done to measure creatinine.
BUN lab test Too Low: Severe liver disease, hepatic
venous shunts (portal-caval shunts), anorexia for several days
(starving, not eating, fasting), pregnancy.
BUN/Creatinine Ratio: This test is used to
differentiate kidney disease from dietary protein metabolism problems.
Considered together, the BUN, blood creatinine and their ratio give very
good evidence of the filtering function of the kidneys and a measure of
the degree of bodily hydration. The ratio of BUN: creatinine is
normally 10:1.
BUN/Creatinine Ratio Too High: Rule out dehydration
(if the ratio is 20:1 or even higher), certain types of kidney disease,
breakdown of blood in the intestinal tract, increased dietary protein,
and any clinical circumstance in which insufficient blood is flowing
through the blood vessels to the kidneys (such as heart failure or
kidney artery disease)..
BUN/Creatinine Ratio Too Low: Rule out certain types of kidney disease, liver disease, malnutrition and Sickle Cell Anemia.
C-Peptide (see under Glucose)
Calcium:
Calcium is controlled in the blood by the
parathyroid glands and the kidneys. Calcium is found mostly in bone and
is important for proper blood clotting, nerve, and cell activity.
Calcium is also found in the bloodstream.
Calcium lab test levels Too High (Hypercalcemia):
Rule out an elevation due to medications such as thiazide-type
diuretics, inherited disorders of calcium handling in the kidneys, diets
containing too much calcium, too many calcium supplements, too much
Vitamin D, multiple myeloma (cancer of the stem cells within the bone
that are responsible for producing all types of red and white cells),
bone cancer, sarcoid, too much protein in the blood, too much albumin in
the blood, fat in the blood (lipemia), excess parathyroid gland
activity such as primary hyperparathyroidism (the thyroid gland has some
kind of tumor or cancer causing the calcium levels to be to high), and
pseudohyperparathyroidism (cancer of the lymphatic system).
Calcium lab test levelsToo Low (Hypocalcemia):
Rule out certain drugs like Fosamax and furosemide-type diuretics, not
enough dietary calcium, not enough dietary Vitamin D, overhydration,
malabsorption, nutritional secondary hypoparathyroidism,
hypercalcitoninism, eclampsia (milk fever?the baby or muscle
contractions during birth have used up too much of the calcium),
pancreatitis with fat necrosis (an infection in the pancreas which has
affected all the extra fat in the body causing it to die from lack of
circulation and nutrition), and not enough protein or albumin in the
blood. Calcium is bound to a particular type of blood protein called
albumin in the blood, so a low albumin level will cause the total
calcium level in the blood to drop in proportion.
Cholesterol:
There are two types of cholesterol, those obtained
from the diet (exogenous) and that produced within the body
(endogenous). Most of the endogenous cholesterol is formed by the liver,
but each cell also produces a little bit as well which makes up part of
the cellular membrane. With just small modifications, cholesterol can
be used as the body needs it as steroids and cholic acid. Cholic acid
uses approximately 80% of the body?s cholesterol, which is converted
into bile?that substance that helps us digest fats. Cutting out
saturated fats from your diet can decrease your cholesterol levels from
15-25%. Eating more unsaturated fats (oils, nuts, seeds) can decrease
your cholesterol. The saturated and unsaturated fats fight for the same
receptor sites on cells. Saturated fats make the cell membranes sluggish
(so you get arthritis and other degenerative diseases) and unsaturated fats make the membranes more liquid so the body works better. (See the Eicosanoid handout: http://naturalhealthtechniques.com/Diet_Nutrition/eicosinoid_survey.htm ) Lack of insulin and thyroid hormones will also increase the cholesterol levels.
Cholesterol is further broken down as follows:
Total Cholesterol: High cholesterol in the blood lab
test is a major risk factor for heart and blood vessel disease.
Cholesterol in itself is not all bad. In fact, our bodies need a certain
amount of this substance to function properly. However, when the level
gets too high, vascular disease can result. Total cholesterol of less
than 200, and an LDL Cholesterol of 100 or less is considered optimal by
the National Heart, Lung, and Blood Institute. As the level of blood
cholesterol increases, so does the possibility of plugging the arteries
due to cholesterol plaque build-up. This is called ?hardening of the
arteries? or atherosclerosis. When the arteries feeding
the heart become plugged, a heart attack may occur. If the arteries
that go to the brain are affected, a stroke occurs.
There are three major kinds of cholesterol, High Density Lipoprotein (HDL) , Low Density Lipoprotein (LDL), and Very Low Density Lipoprotein (VLDL). The lower the density of cholesterol, the more cholesterol molecules there are.
HDL (High Density Lipoprotein)
cholesterol is a ?good cholesterol? as it protects against heart disease
by helping remove excess cholesterol deposited in the arteries. High
levels in the lab test seem to be associated with low incidence of
coronary heart disease.
LDL (Low Density Lipoprotein)
cholesterol is considered to be ?bad cholesterol? because cholesterol
deposits form in the arteries when LDL levels are high. LDL levels of
less than 130 are recommended. One hundred is optimal and values greater
than 160 are considered high risk. Those persons who have established
coronary or vascular disease may be instructed by their doctor to get
their LDL cholesterol well below 100. You should ask your doctor which
LDL target he or she wants for you-but do some of your own research as
well.
There are two ways to report LDL. The most common is simply an
estimate calculated from the Total Cholesterol, HDL, and triglycerides
results. This may read ?LDL Calc? on your lab test
results. A directly measured LDL cholesterol is usually more accurate,
but more expensive and may require that your doctor specify the Direct LDL test.
VLDL (Very Low Density Lipoprotein: This is the only
lipoprotein initially formed in the liver and contains mostly
triglycerides and very little phospholipids and cholesterol. As they
flow through the blood vessels they are quickly broken up and used as
energy or stored as fat.
Cholesterol lab test Too High: Rule out
hypothyroidism, obstructive jaundice, liver disease, nephrosis, diabetes
mellitus, familial, pancreatitis, hyperadrenocorticism, diet, retained
anger and resentment.
Cholesterol Too Low: Rule out hyperthyroidism,
infection, malnutrition, heart failure, malignancies, low fat diet,
intestinal malabsorption and hepatic insufficiency.
Creatinine. (Also known as Creatine phosphokinase, CK and CPK)
CPK is an enzyme which is very useful for diagnosing diseases of the
heart and skeletal muscle. This enzyme is the first to be elevated after
a heart attack. If CPK is high in the absence of heart muscle injury,
this is a strong indication of skeletal muscle disease. Most creatinine
is produced in the muscle, heart and brain. Creatinine is a
water-soluble waste product largely from muscle breakdown that is
excreted via the kidney tubules. Creatinine is not affected by the
amount of urine produced and excreted. When creatinine breaks down it
gives us energy because it acts as an enzyme important in the process of
forming ATP (that very basic process that gives us energy).
The rule outs for too high and too low creatinine levels in the lab test are the same as for BUN
(Blood Urea Nitrogen): If the kidneys are not functioning properly, the
concentrations of creatinine and blood urea nitrogen will rise in the
blood. The laboratory uses the blood urea nitrogen (BUN) and creatinine
levels to assess kidney function. In addition, a urinalysis is used to
measure kidney output function and health of the collecting system
(lower portion of kidney, ureters and bladder).
Creatinine lab test Too High: Rule out dehydration,
too much exercise, hemorrhagic shock (shock due to too much blood being
lost), pancreatitis, intestinal foreign body, too much protein in the
diet, bleeding within the intestine, drugs like amphotericin B,
hyperthyroidism (humans) and hypothyroidism (animals-sometimes), adrenal
cortical insufficiency (adrenal glands not producing enough of the
hormones it is suppose to be producing), any condition which decreases
blood flow to the kidneys such as, glomerulonephritis (the little
tubules that make the urine in the kidneys are swollen and not working
right), amyloidosis (the kidney tissue is being replaced with some kind
of unnatural protein), pyelonephritis (inflammation/infection of the
kidney where the urine pools before it dumps out into the ureters),
nephrosis (a condition of the kidneys), calcium nephropathy?also called
lymphosarcoma (cancer of the kidneys where the tissues are being
replaced by calcium so the urine can?t get out and so it builds up in
the body instead), kidney cancers, obstruction of the urine coming out
of the kidney, ruptures of the urine carrying parts (kidney, ureters,
bladder, urethra, kidney tubules.
Creatinine lab test Too Low: Rule out severe liver
disease, hepatic venous shunts (portal-caval shunts), anorexia for
several days (starving, not eating, fasting), and pregnancy.
GGT (Gamma glutamyltransferase or Gamma glutamyl transpeptidase)
GGT is an enzyme that is in high levels specifically
in kidney tubule cells and in bile producing cells of the liver. When
it shows up in high levels in the blood serum, it is of liver origin.
When it if from the kidneys, a special test needs to be run to see it,
so this one can be missed because it is not a part of routine blood
work.
GGT Too High: Rule out liver disease, particularly
with obstruction of the bile ducts (cholestasis) and in acute hepatic
necrosis (liver cells dying and rotting very quickly). Unlike alkaline
phosphatase it is not elevated with bone growth or damage.
C-peptide :
C-Peptide is a fragment cleaved off of the precursor of insulin
(pro-insulin) when insulin is manufactured in the pancreas. C-peptide
levels usually correlate with the insulin levels, except when people
take insulin injections. When a patient is hypoglycemic, this test may
be useful to determine whether high insulin levels are due to excessive
pancreatic release of insulin, or from an injection of insulin.
LDH (Lactate Dehydrogenase)
LDH is the enzyme present in all the cells of the
body. Anything that damages cells, including blood drawing itself, will
raise amounts in the blood. If blood is not processed promptly and
properly, high levels may occur.
Lactate Dehydrogenase Too High: Rule out heart
attack, pulmonary infarction, hemolytic anemia, pernicious anemia,
leukemia, lymphoma, malignancies, renal infarction, seizures, cerebral
damage, trauma, sprue (a chronic intestinal malabsorption disorder
caused by gluten intolerance), lymphosarcoma, lipemia (fat in the
bloodstream), improper sample handling (broken cells), necrosis (tissue
death) of the liver, skeletal muscle, kidney, pancreas and myocardium
and using old blood samples for running the test.
Note: If all values except LDH are within expected ranges, it is probably a processing error and does not require further evaluation.
Lactate Dehydrogenase Too Low: Not clinically significant.
Phosphorus:
Phosphorus is a mineral largely stored in the bone and is regulated by the kidneys.
Phosphorus Too High (Hyperphosphatemia): Rule out
kidney disease, normal in young animals, high protein diets, too much
Vitamin D, hypoparathyroidism, diabetic acidosis, acromegaly, Addison?s
disease, calcium nephropathy, lymphosarcoma (if BUN is also elevated),
and not allowing the blood tube to clot before separating the serum from
the sample before mailing.
Phosphorus Too Low (Hypophosphatemia): Rule out
inadequate diet, malabsorption, parathyroid conditions such as primary
hyperparathyroidism and pseudohyperparathyroidism, Vitamin D deficiency,
osteomalacia, rickets, Fanconi syndrome, cirrhosis, hypokalemia, excess
IV glucose, too much insulin in the system (either from injection or
cancer of the pancreas). When low levels of phosphorus are seen with
high levels of calcium it suggests parathyroid disease.
Potassium:
Potassium is an essential mineral controlled very
carefully by the kidneys. It is important for the proper functioning of
the nerves and muscles, particularly the heart. Any value outside the
expected range, high or low, requires medical evaluation. This is
especially important if you are taking a diuretic (water pill) or heart
pill (Digitalis, Lanoxin, etc.).
Potassium Too High (Hyperkalemia): Rule out
Addison?s disease (adrenal cortical insufficiency), dehydration, cardiac
arrhythmia, severe renal disease, hyperkalemic acidosis, diabetic
acidosis, hypoadrenalism, hereditary hyperkalemia, metabolic acidosis
(like in diabetes mellitus).
Note: Hemolyzed blood will also
cause a slight increase in potassium because 85% of all the potassium in
the body is stored within the cells. Hemolyzed blood can happen when
the sample is damaged and the blood cells have broken in the process of
either collecting the sample or in handling the vials during transport
to the lab. I have also seen it occur when the syringe is pulled back
too quickly or too far causing the vein to collapse (impatience). This
doesn?t happen often in humans because a needle is inserted into the arm
vein and the tube pushed onto the needle. In this way the blood does
not suck into the tubes too quickly and the sample stays intact (animals
are not that cooperative, so that?s another story).
Potassium Too Low (Hypokalemia): Rule out cirrhosis,
malnutrition, metabolic alkalosis, nephrosis, hyperadrenalism, familial
periodic paralysis (need DNA testing for this), overhydration with
potassium low fluids, diarrhea, vomiting, intestinal obstruction,
malabsorption, Cushing?s disease, insulin treatments driving potassium
into the cells, drugs such as mercurial diuretics and
hydrochlorothiazide (blood pressure medications).
Sodium:
Sodium is an essential mineral regulated by the kidneys and adrenal glands and present in every cell of our body.
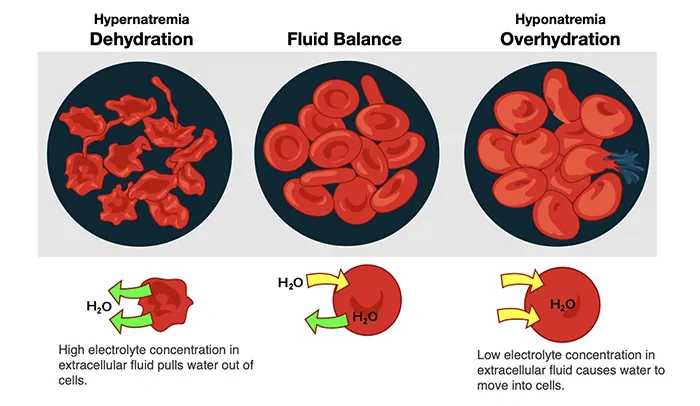
Sodium Too High (Hypernatremia): Rule out
dehydration, heart disease, salt poisoning, eating too many salty foods,
faulty water softener dumping too much salt into the water, and
diabetes insipidus.
Sodium Too Low (Hyponatremia): Rule out Addison?s
disease (adrenal cortical insufficiency), diarrhea, overhydration with
fluids not containing salt, malabsorption, diabetic acidosis, severe
renal disease, ruptured or obstructed urinary system, overdose of
certain drugs such as diuretics and blood pressure medications (like
hydrochlorothiazide), excess antidiuretic hormone, nephrosis,
hypoadrenalism, myxedema, congestive heart failure, vomiting, diabetic
acidosis, and excessive water intake in patients with heart or liver
disease.
Total Protein (TP):
Total protein in the blood includes clotting
factors, enzymes, antibodies, transport substances, albumin and most of
the alpha and beta globulins. Total protein is measured in
grams/deciliter with an instrument called a refractometer. A
refractometer is a machine that can measure how much light passes
through a substance.
Protein Too High (Hyperproteinemia): Rule out
dehydration, too much albumin and fibrin, globulin increases from
tissue injury, inflammation, active liver disease, strongylosis
(roundworm infestation), immune-mediated disease, lymphoid neoplasms,
and myelomas (bone cancer). Factors giving false elevations include
abnormally high concentrations of glucose, urea, sodium, chloride or
lipids. Hemolysis (but not icterus) also causes mild elevations.
Protein Too Low (Hypoproteinemia): Rule out decreased production, intestinal malabsorption, malnutrition, exocrine pancreatic insufficiency,
chronic liver disease, accelerated loss of protein, hemorrhage, renal
disease (proteinuria), protein-losing enteropathies, severe exudative
skin disease, burns, high-protein effusions, hepatic insufficiency,
colostrum deprivation, combined immunodeficiency (foals),
agammaglobulinemia, selective IgM deficiency, transient
hypogammaglobulinemia, and Disseminated Intravascular Coagulation (DIC).
Triglycerides (also called Neutral Fat):
Triglycerides (along with carbohydrates) are fats in the blood used
in the body mainly to provide energy for the different metabolic
processes. Those that are not used for energy are quickly stored as fat.
Triglycerides Too High: Rule out post-prandial (just
after eating they go up), heart disease (severe elevations), endocrine,
hepatic, pancreatic and renal disease, high-fat diets, low insulin,
hypothyroid, heparin injections, diabetes mellitus, and exogenous
corticosteroids.
Uric Acid:
Uric Acid is a breakdown product of nucleic acids
normally excreted in urine. Nucleic acids make up the components of DNA
and RNA in our bodies.
Uric Acid Too High: Rule out gout,
arthritis, kidney problems leukemia, lymphoma, polycythemia, acidosis,
psoriasis, hypothyroidism, eclampsia, multiple myeloma, pernicious
anemia, tissue necrosis, inflammation, and the use of some diuretics.
Uric Acid Too Low: Rule out uricosuric drugs (drugs
that break down uric acid and assist it to leave via the urine?as your
pharmacist on this), too much allopurinol (the drug used in the
treatment of gout), Wilson?s Disease (a genetic disease of the liver
which allows copper to build up to toxic levels), and large doses of
Vitamin C.
Bile Acids:
Bile acids produced by the liver cells. They are bound by the amino
acids glycine or taurine and then dumped into the bile. Bile acids help
us to digest our foods?especially the fatty ones. Sometimes I see people
(and cats) that have vision problems and enlarged hearts who test out
as having taurine deficiency so there may be an association. I don?t
know for sure.
Bile Acids Too High (Increased bile acids): Rule out
blocked bile ducts (gall stones?), acute toxic hepatic necrosis,
anicturic liver disease, alcoholic liver disease, biliary atresia,
chemical and drug induced liver injury, cirrhosis, cholestasis, cystic
fibrosis, generalized pruritus (itchy rash all over the body), hepatoma,
nausea and vomiting associated with pregnancy, neonatal hepatitis,
protracted diarrhea in infants, Reye?s syndrome, and viral hepatitis.
Bile Acids Too Low: Not clinically significant.
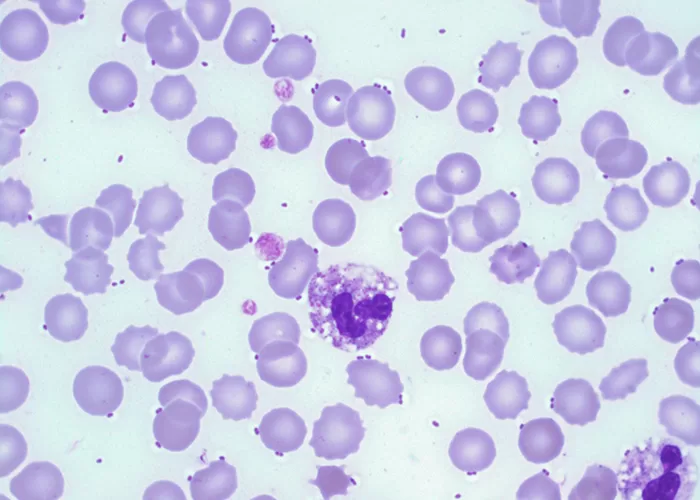
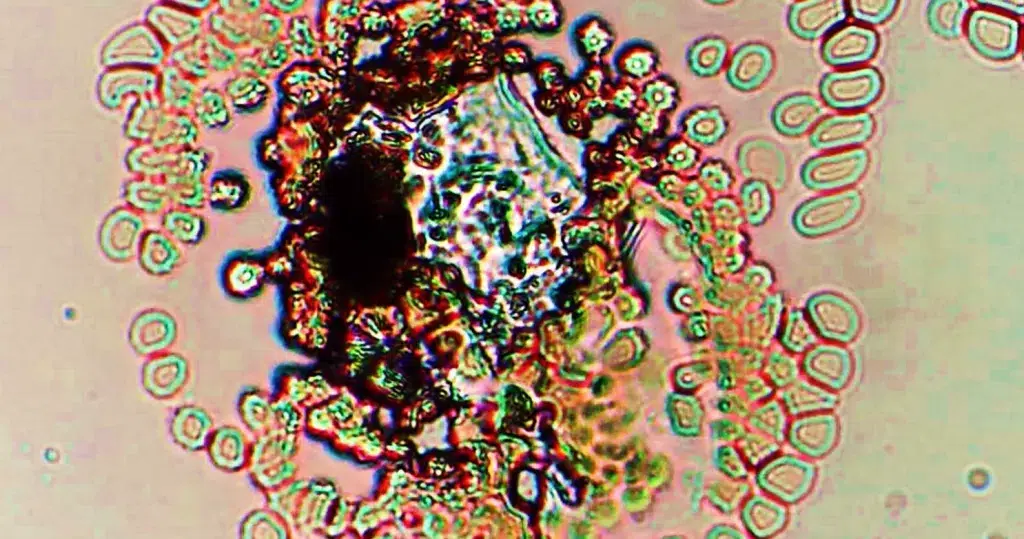
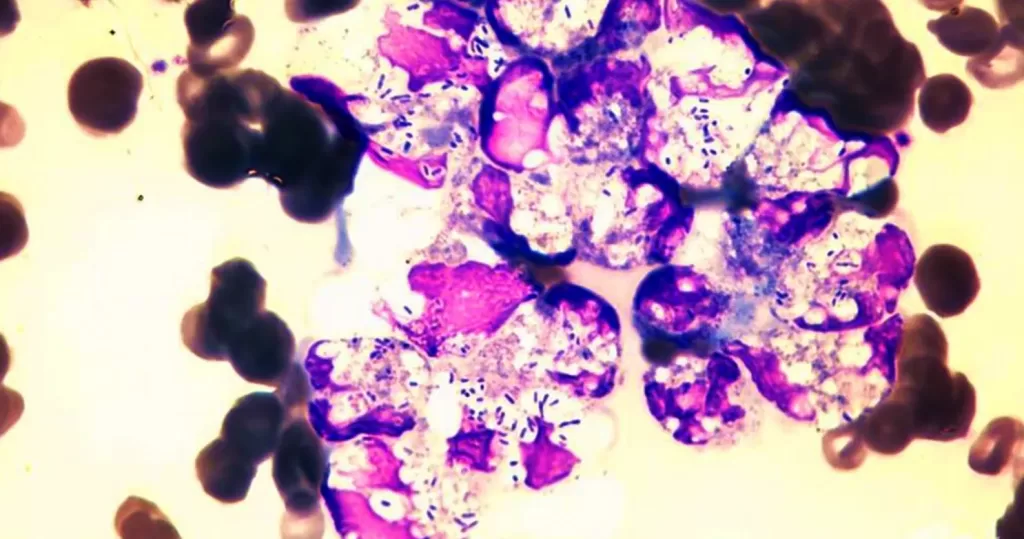
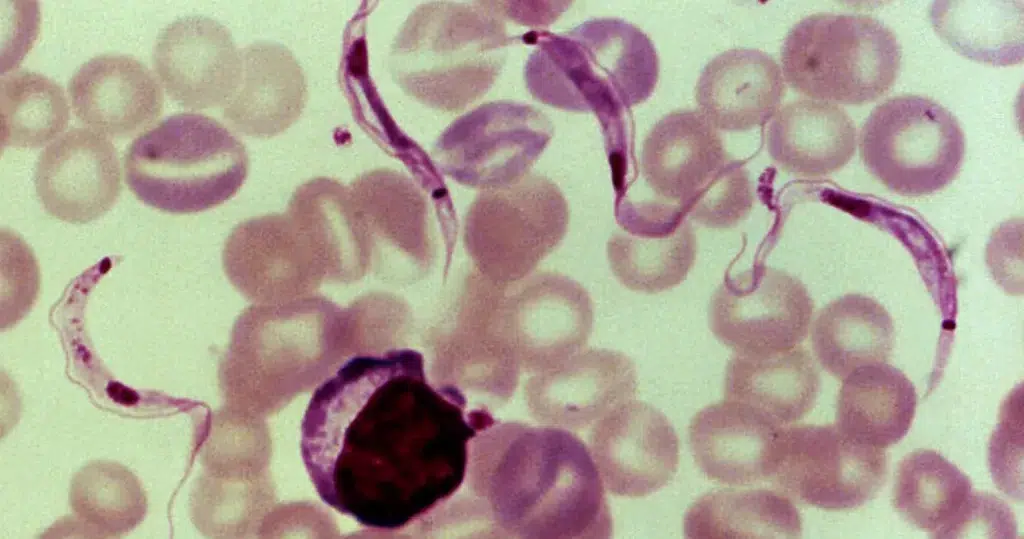
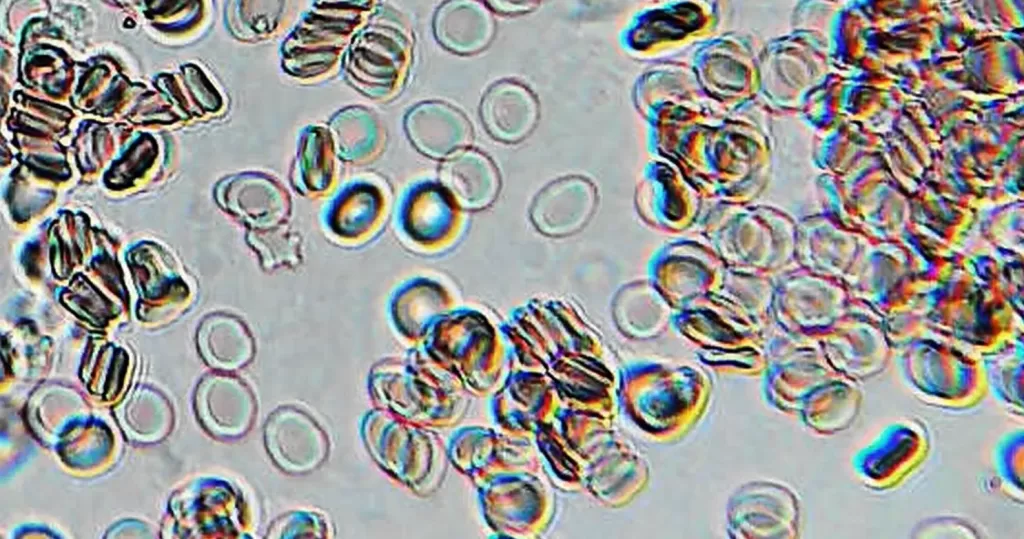
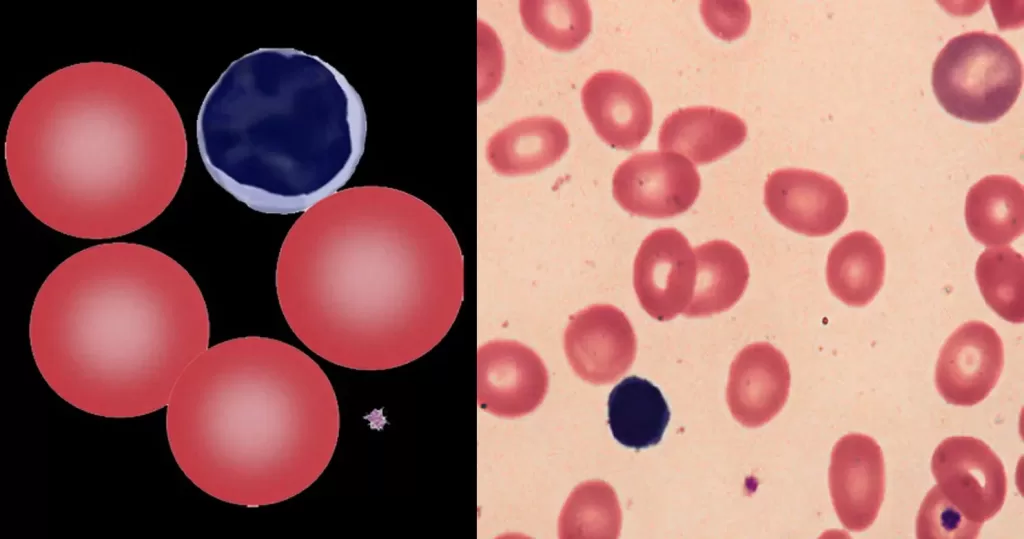
Complete Blood Count (CBC):
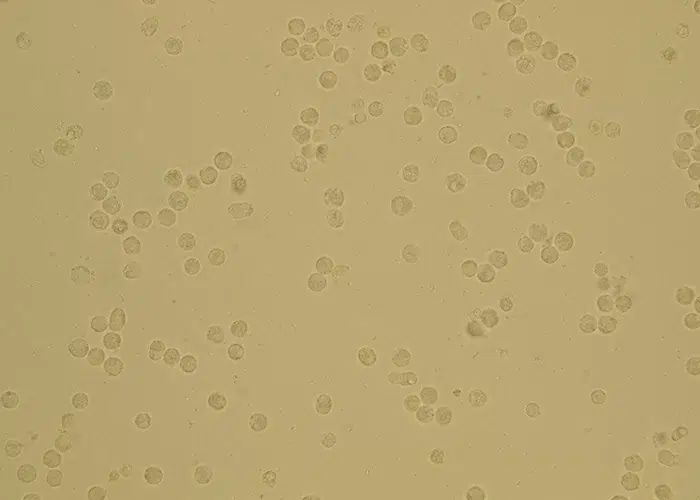
When all the cellular components of the blood are looked at and characterized as to their numbers this is called a Complete Blood Count or CBC. Within the CBC the white cells, red cells and platelets are counted. A white cell count is called a WBC (White Blood Cell count) and a red cell count is called an RBC (Red Blood Cell count). The CBC typically has several parameters that are created and evaluated using an automated cell counter. These are the most relevant:
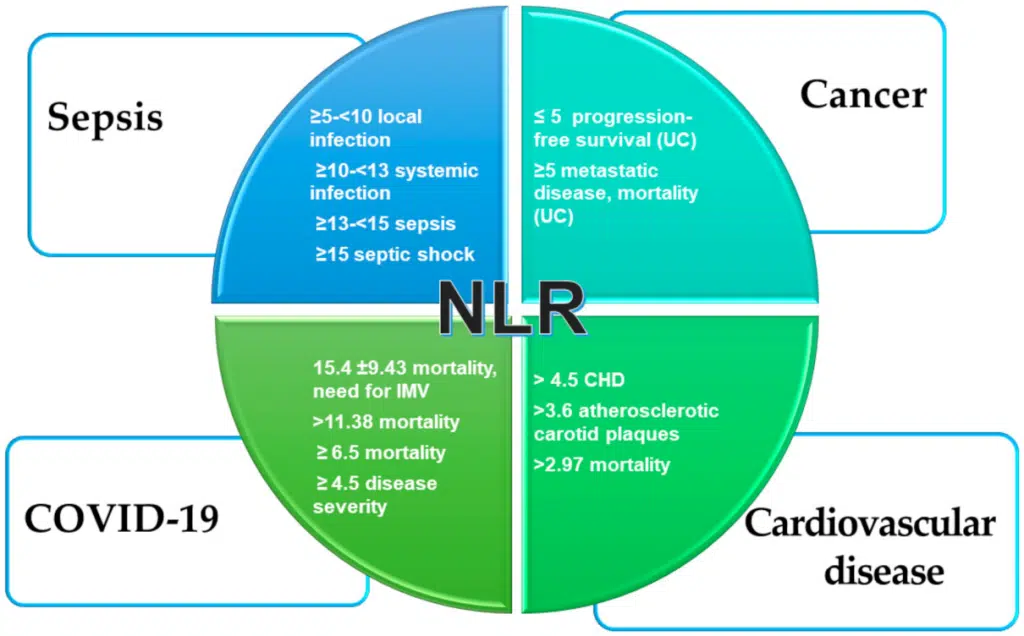
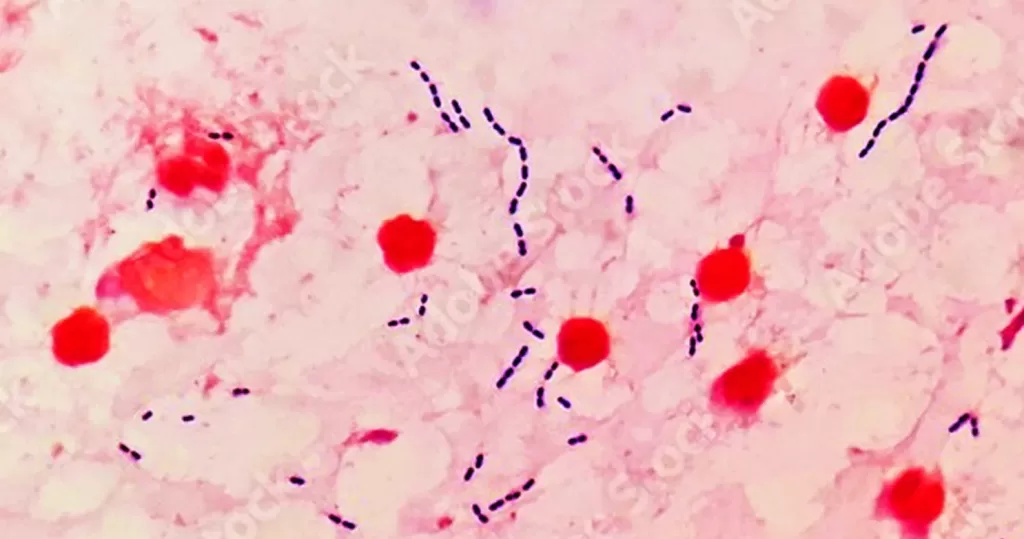
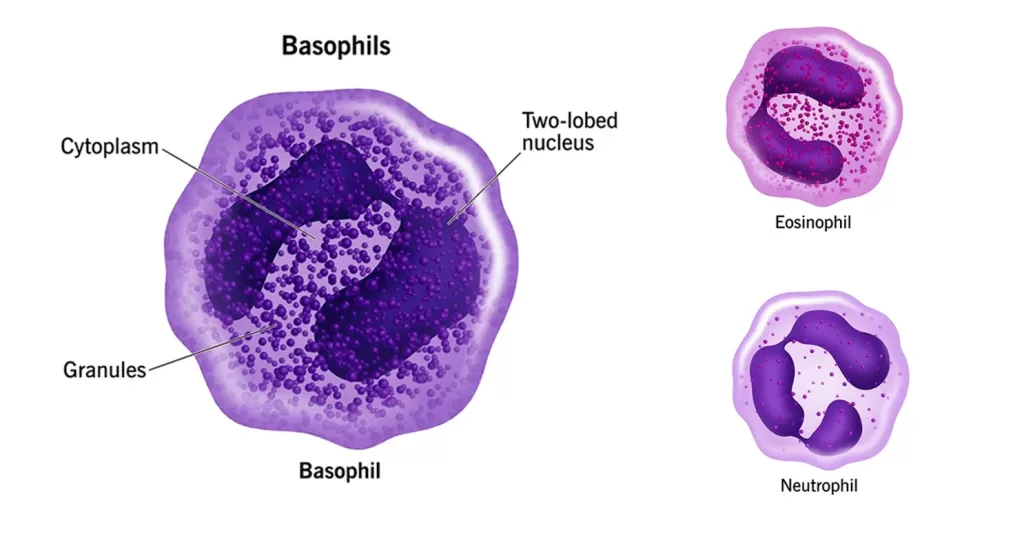
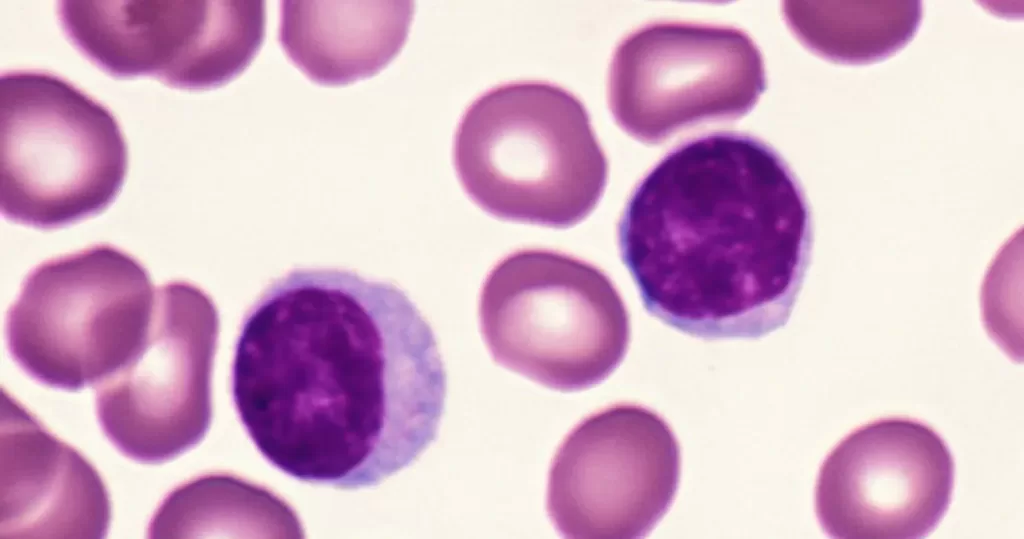
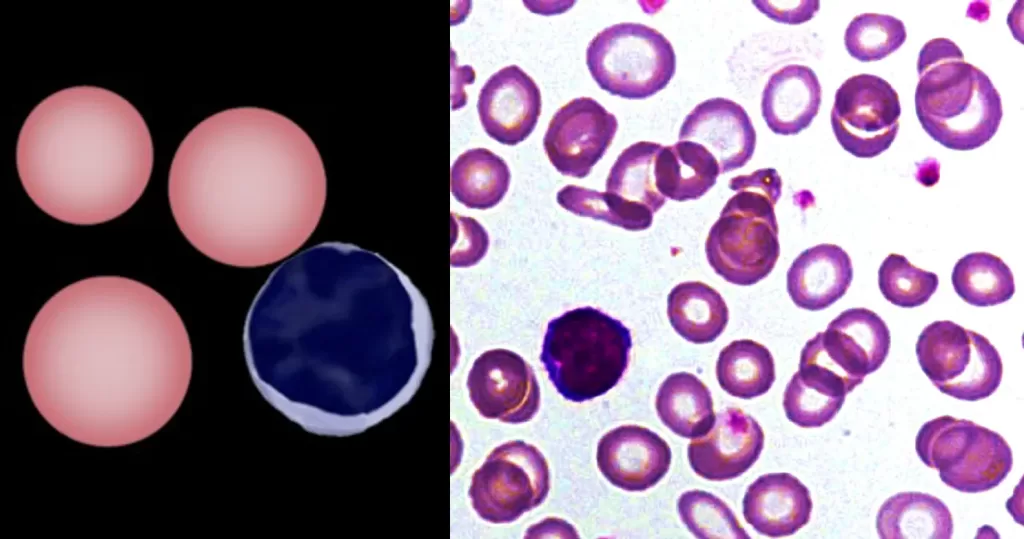
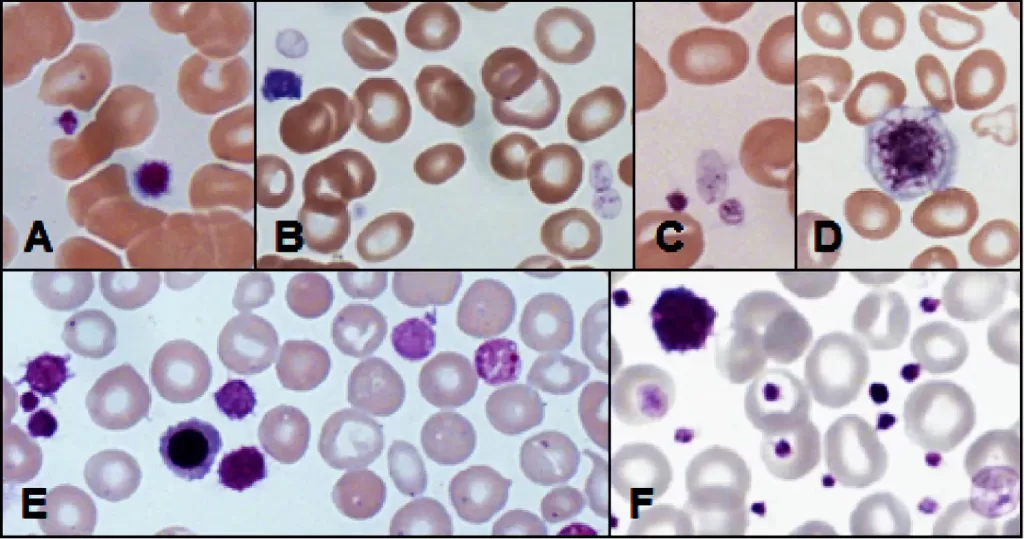
WBC (White Blood Count)
White blood cells are responsible for detecting and destroying
diseases that come into our body. There are several ways to measure
white blood cells. White cells are also broken down into their
individual categories of types of cells that fight different things.
These include Neutrophils, Lymphocytes, Monocytes, Eosinophils, and Basophils.
Most times these cells are counted by automation (machine), but
sometimes the doctor would like to see the character of the cells to
detect any differences that the machine can?t detect with it?s
mechanism, so a hand count is done and abnormalities noted.
White Blood Count Too High: Rule out infection and leukemia.
White Blood Count Too Low: Rule out bone marrow
diseases or an enlarged spleen, pooling of the cells within the body
(like in pyometra), HIV (Note: The vast majority of low WBC counts in
our population is NOT HIV related.)
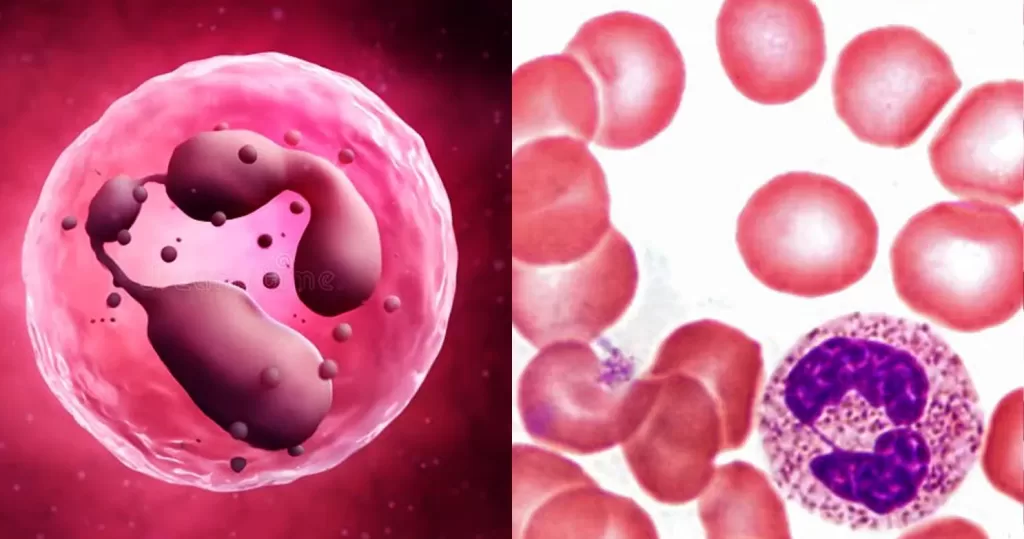
Neutrophils:
Neutrophils are a type of white blood cell that
circulate in both tissues and blood. They act like little ?Pac Men? in
the tissues finding bacteria and chomping them up. Once they move from
the circulation into the tissues, they don?t return. They are replaced
two times or more each day, so you can see that these cells can really
multiply when there is a problem.
Neutrophils Too High on the CBC lab test: Rule out
stress, pain, very high or very low body temperatures (which cause
cortisol to be released from the system), drugs such as cortisone,
strenuous exercise, bacterial infections (cat bite abscesses are a
fabulous representation of this!), increased heart rate and increased
blood pressure. When neutrophils increase with stress (called a stress
leukogram), the neutrophil count goes up and the leukocyte count
decreases at the same time.
To Read about Gout go to: http://naturalhealthtechniques.com/SpecificDiseases/gout1.htm
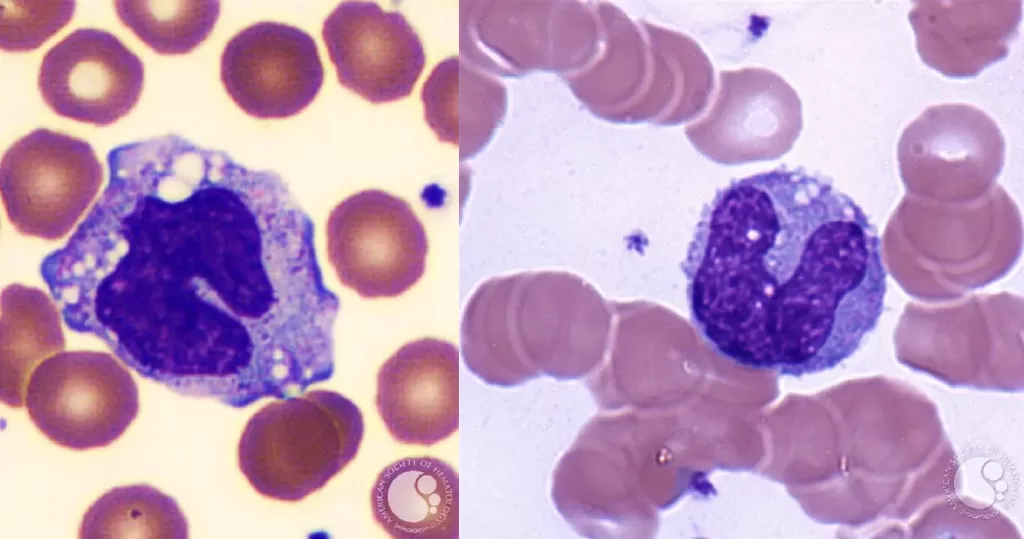
Lymphocytes:
Lymphocytes live in the immune rich tissues like the
lymph nodes, spleen, tonsils, thymus, gastrointestinal lymphoid tissue,
bronchial lymphoid tissue, bone marrow and in the blood. There are lots
of lymph nodes in the breast, under the arm, behind the knees, in the
neck, and in the groin areas. Lymphocytes are specifically attracted to
viruses, pollens and cells that have anything wrong on them on the
outside of the cell (this is called cell-mediated immunity).
They live a lot longer (weeks) than neutrophils and DO recirculate from
the tissue to the blood and back. They go where they are needed.
Lymphocytes are further broken down into T-cells, and B-cells, but
special testing is needed to determine how much of each we have.
T-cells:
T-cells have the ability to never forgive and never
forget. When they detect something bad in the system they attack it. If a
particular T cell was programmed to attack the cancer virus, it will
always attack cancer virus (and not much else). Sometimes these
particular cancer-attacking white cells are called ?Killer cells?.
We stimulate our immune system to train the T-cells by using vaccines,
homeopathic nosodes, and exposing ourselves to infectious agents. This
makes our immune system strong.
B-cells:
B-cells wait around for orders. They will turn into T
cells if necessary, but most times their job is to produce antibodies.
Antibodies glom onto foreign substances that get into the body and they
remove it. When antibodies get the wrong orders (like when a person is
highly allergic to bee stings), the B cells sometimes overreact or react
too quickly causing anaphylactic shock.
Lymphocytes:
Lymphocytes Too Low (Lymphopenia): Rule out
corticosteroids, stress, pain, acute systemic infections (viral and
bacterial), acquired T lymphocyte deficiency (neonatal infections),
immunosuppressive drugs, irradiation, loss of lymph, chylous thoracic
effusion (ruptured thoracic duct), lymphosarcoma, enteric neoplasms,
granulomatous enteritis, Johne?s disease (cattle), protein-losing
enteropathies, ulcerative enteritis, lymphatic cancer destroying lymph
nodes, and hereditary T-cell deficiency.
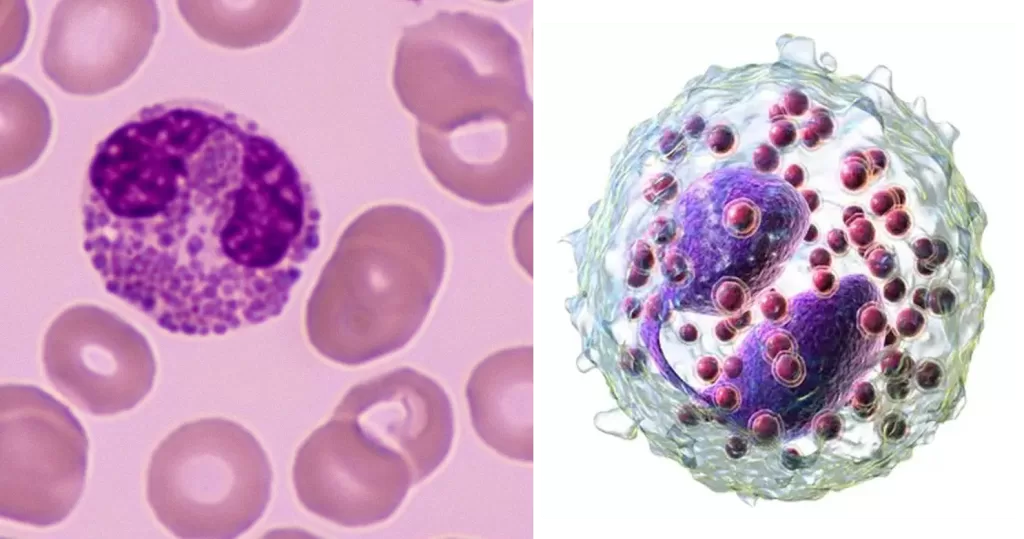
Monocytes:
Monocytes can be elevated (monocytosis)
in response to corticosteroids, with pus conditions (abscesses),
necrosis, malignancy, hemolysis, hemorrhage, mononucleosis, immune
injury, pyogranulomatous diseases, and in acute and chronic stages of
disease.
Eosinophils:
Eosinophils are elevated (eosinophilia)
with parasite infestation, allergies, myositis, canine and feline
eosinophilic granuloma complex, eosinophilic gastroenteritis,
panosteitis, milk sensitivity (cattle), feline staphylococcal or
streptococcal infections and mast cell neoplasia.
Basophils:
Basophils are the least numerous of the white blood cells. Observing even a few cells on the blood smear usually attracts attention.
Basophils Too High (Basophilia): Rule out parasites,
hypersensitivities, heartworm (without microfilaria in the blood),
altered plasma lipoprotein metabolism causing endocrine diseases,
nephrotic syndrome, chronic liver disease, genetic
hyperlipoproteinemias, and mastocytomas (Mast cells look much like
basophils).
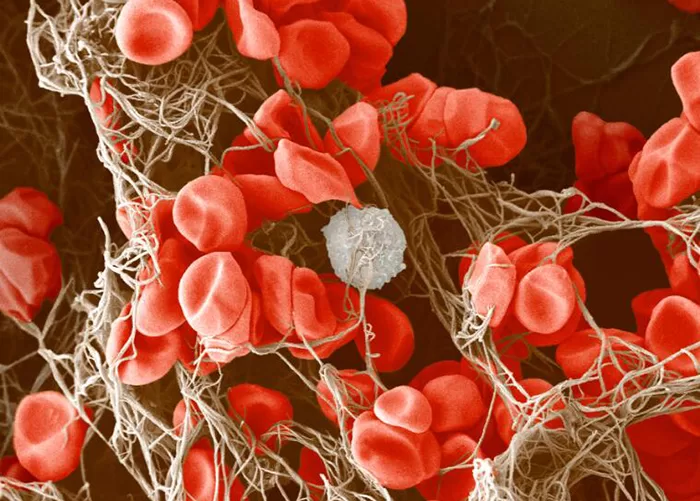
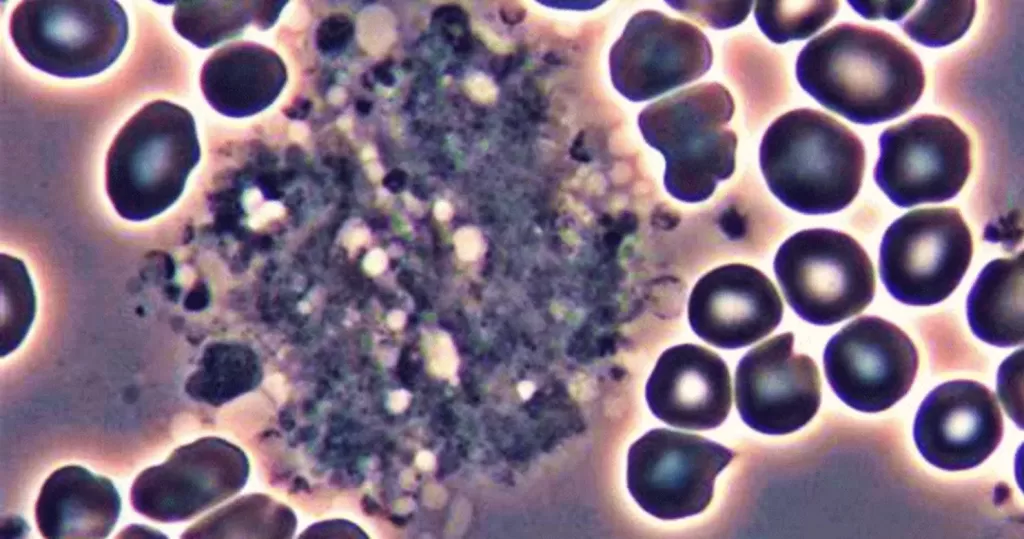
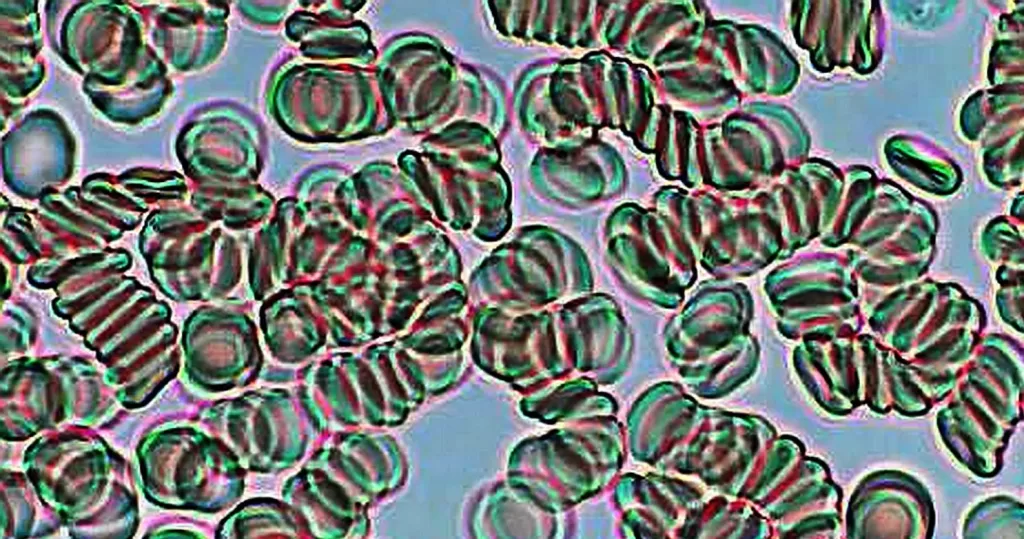
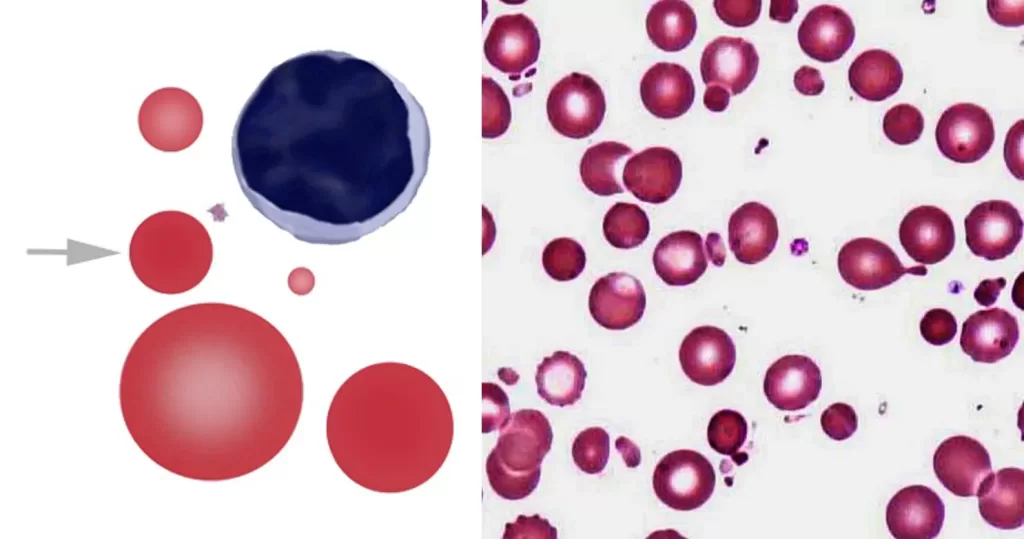
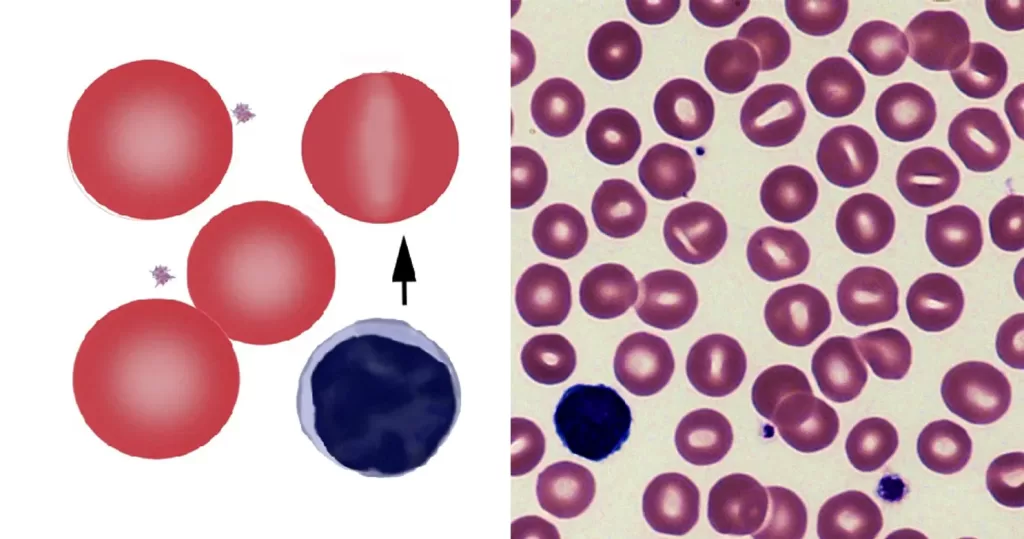
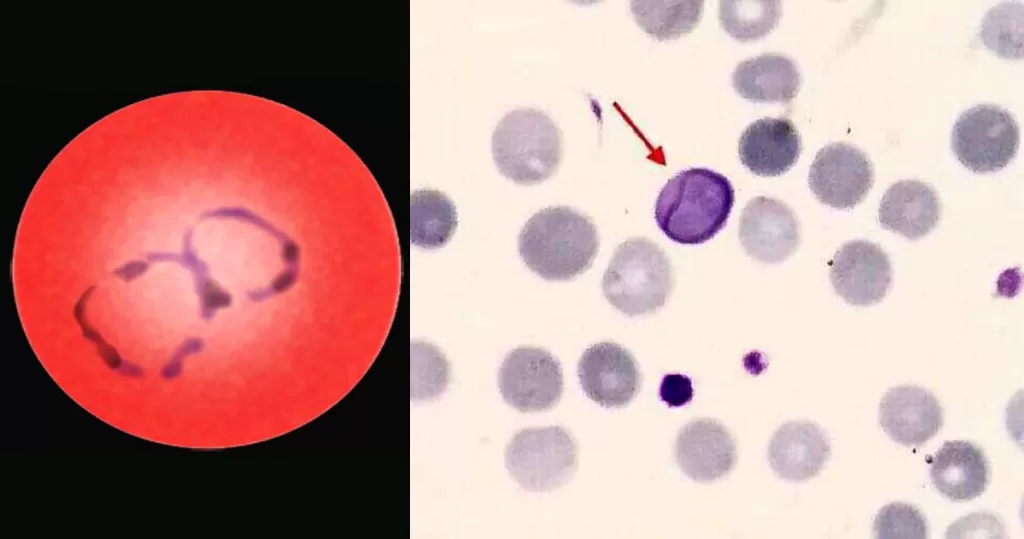
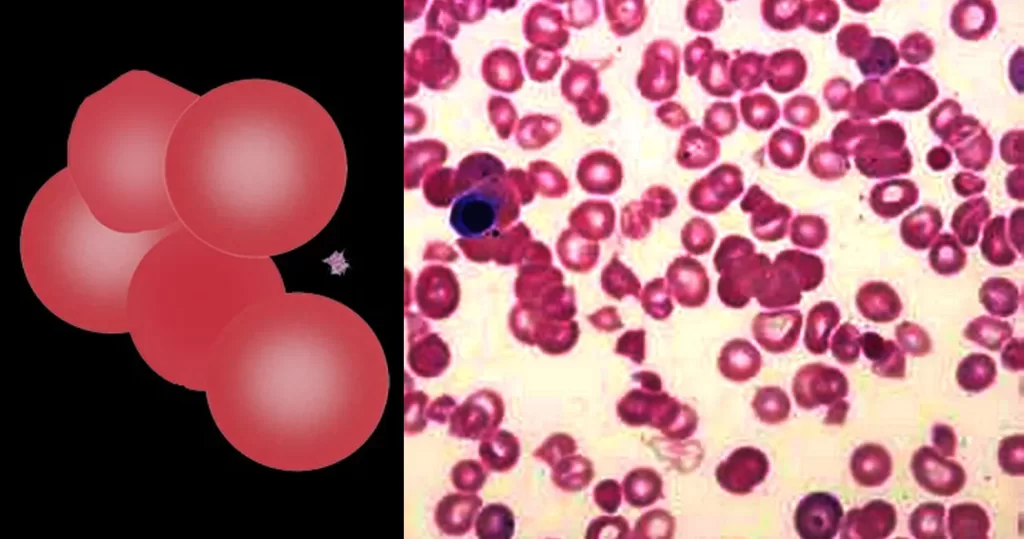
Platelet Count (PLT or Thrombocyte count):
Platelets are cells that plug up holes in blood vessels and prevent
bleeding. This test measures the number of platelets in a drop
(microliter) of blood. Normal values range from 150,000 to 400,000
platelets per microliter. A count below 50,000 can result in spontaneous
bleeding; below 5,000, patients are at risk of severe life-threatening
bleeding.
Platelet Count Too High (Thrombosis): Rule out
bleeding, cigarette smoking, excess production by the bone marrow,
strenuous activity, myeloproliferative disorders, infections,
inflammation, cancers, and when the spleen has been removed.
Platelet Count Too Low (Thrombocytopenia): Rule out
premature destruction states such as immune-mediated thrombocytopenia,
acute blood loss, drug effects (such as heparin), infections with
sepsis, entrapment of platelets in an enlarged spleen, or bone marrow
failure from diseases such as myelofibrosis or leukemia. Platelet counts
decrease just before menstruation. If there are not enough platelets in
your blood, you may notice signs of bleeding such as nosebleeds, easy
bruising, prolonged bleeding from a cut, black or bloody stools, brown
or red urine, or tiny pinpoint sized red or purple spots on your skin,
under your nails or in your gums (petechial hemorrhage). Low platelets
also can occur from clumping of the platelets in a lavender-top tube.
You may need to repeat the lab test with a green top tube in this case.
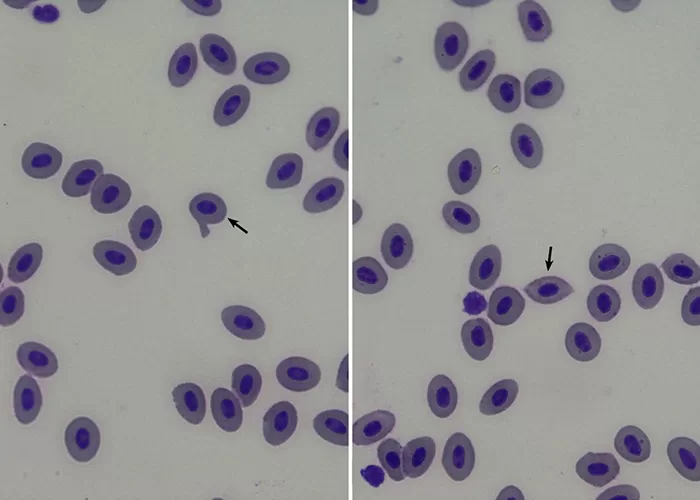
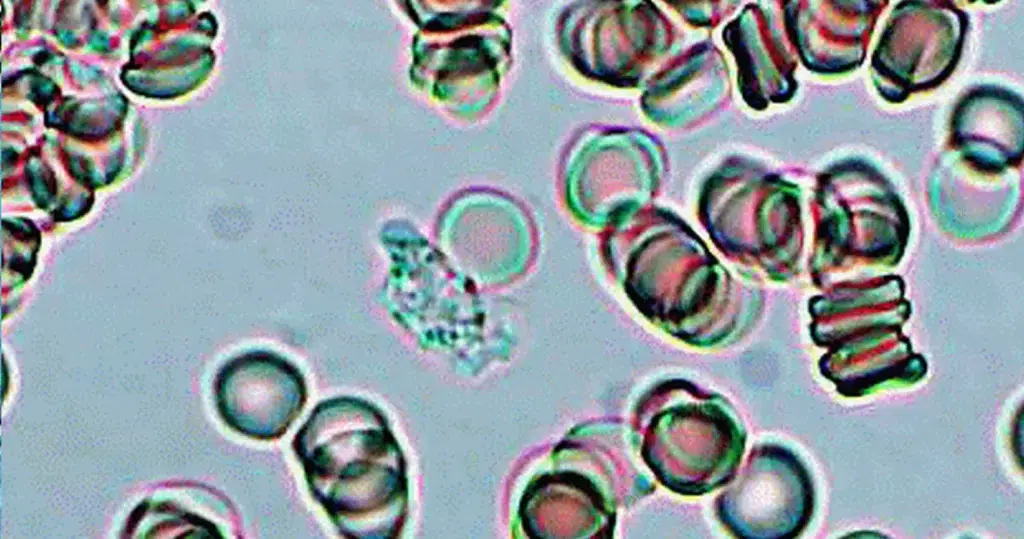
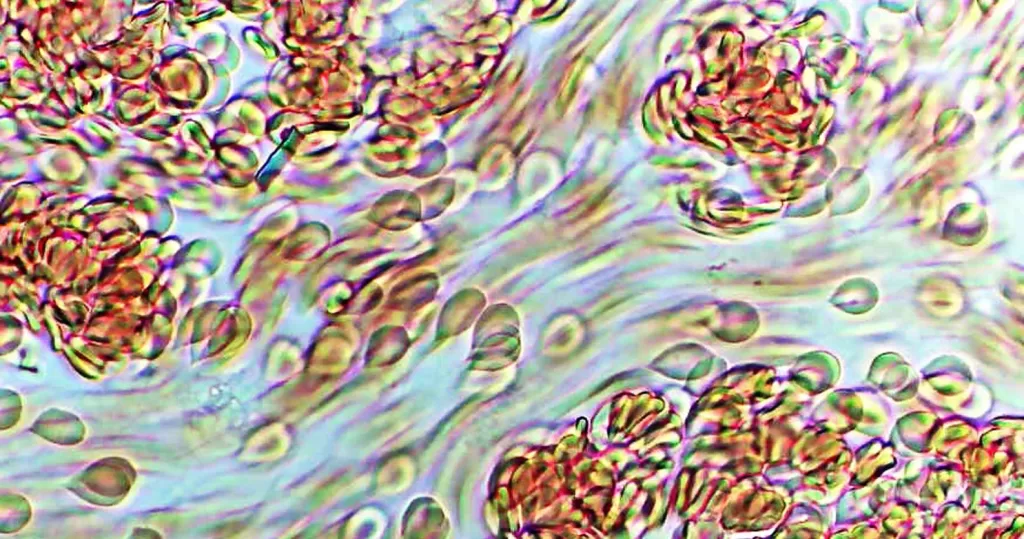
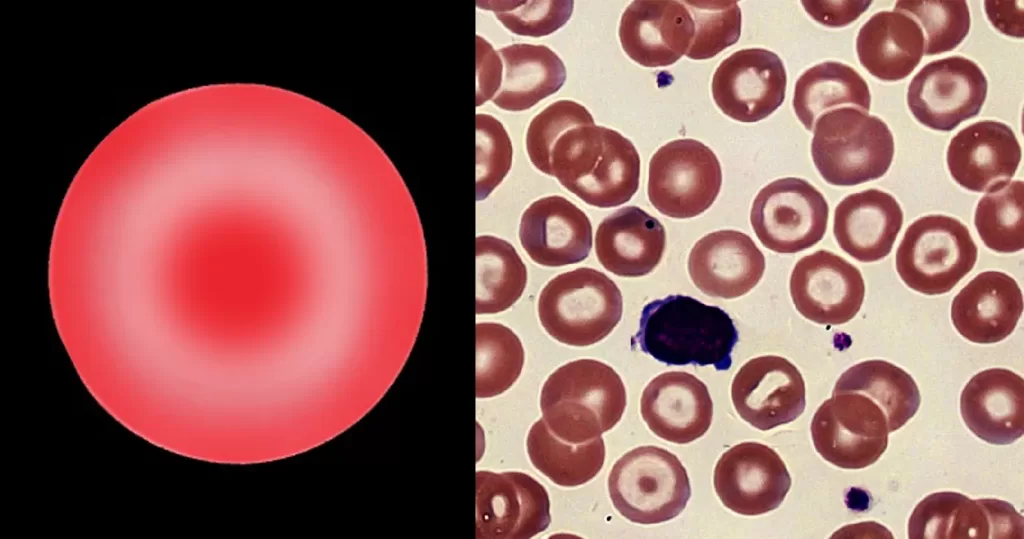
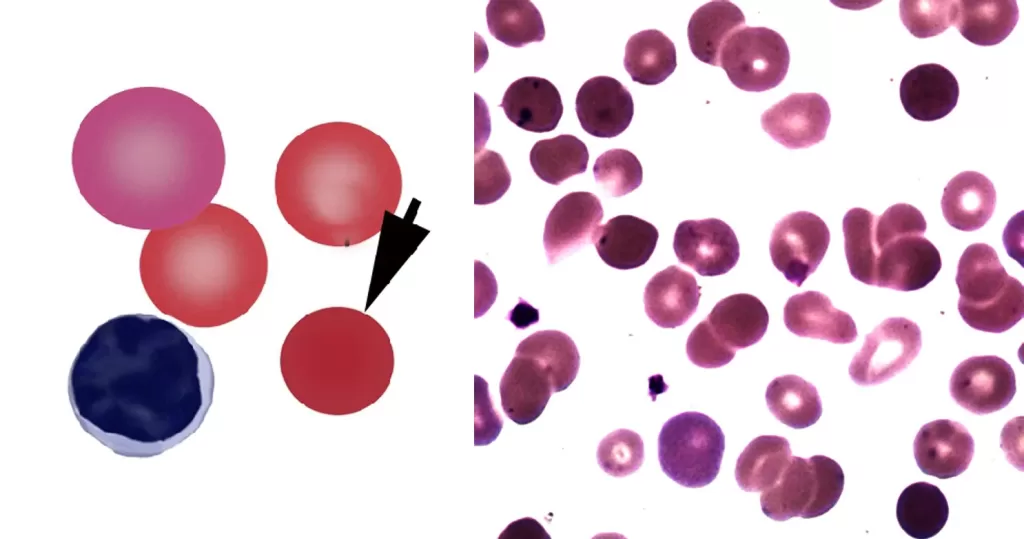
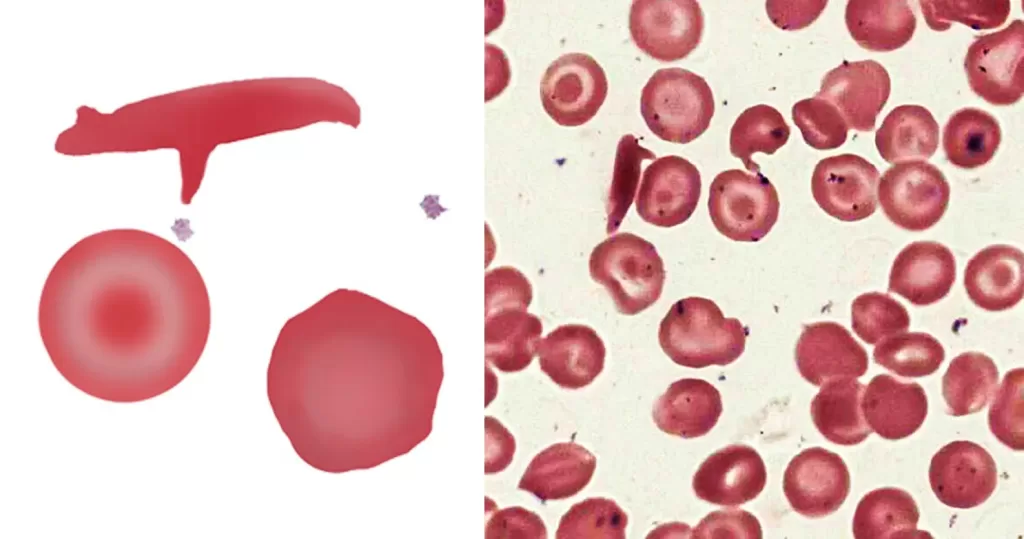
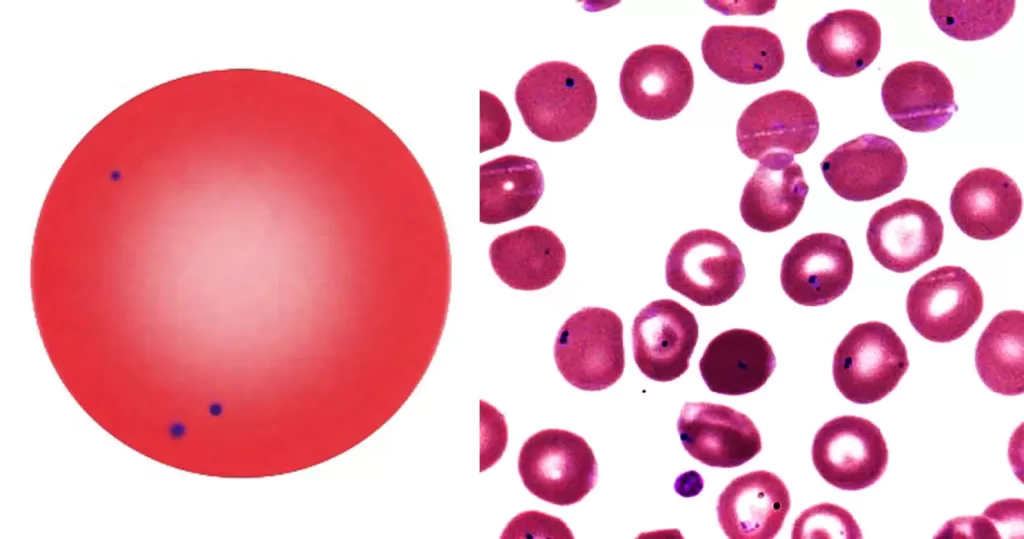
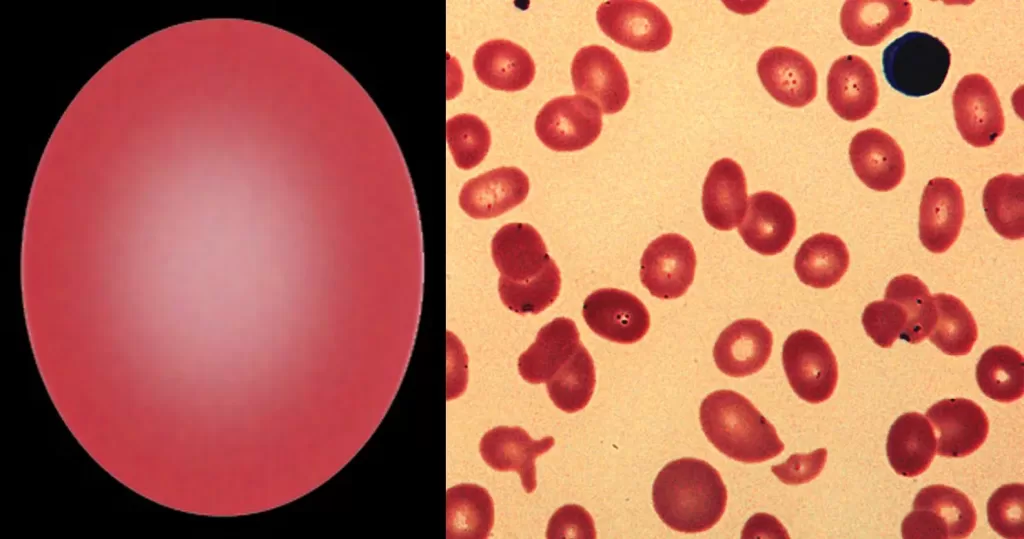
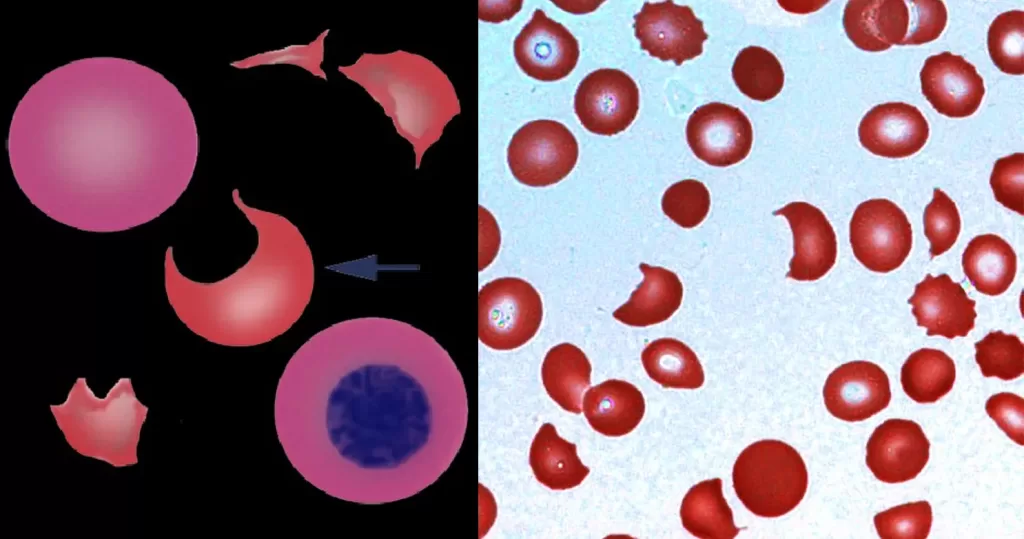
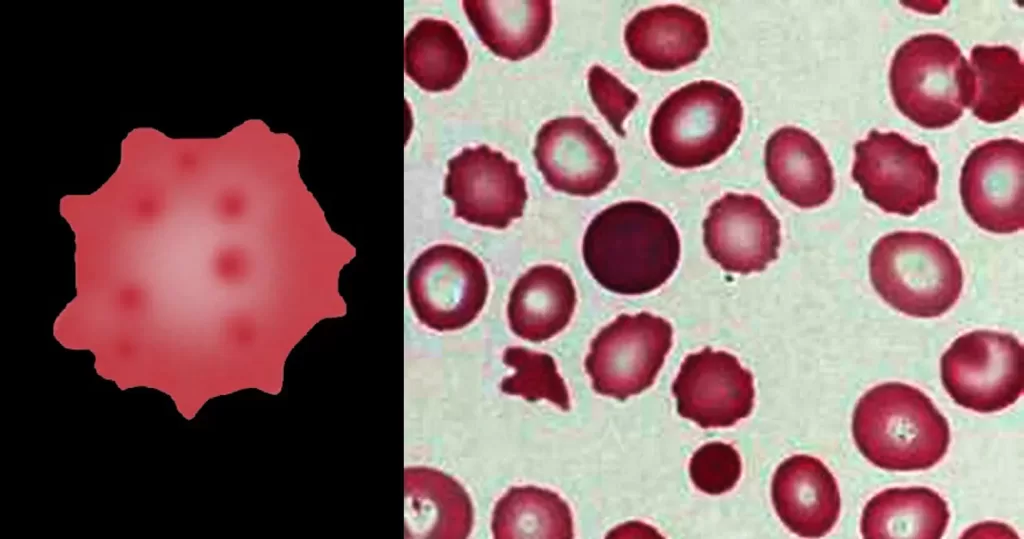
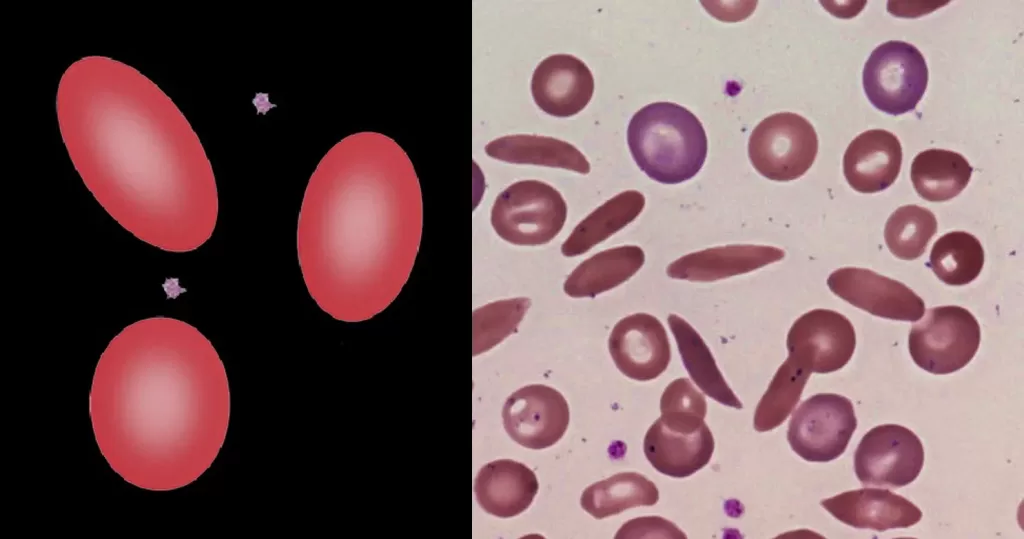
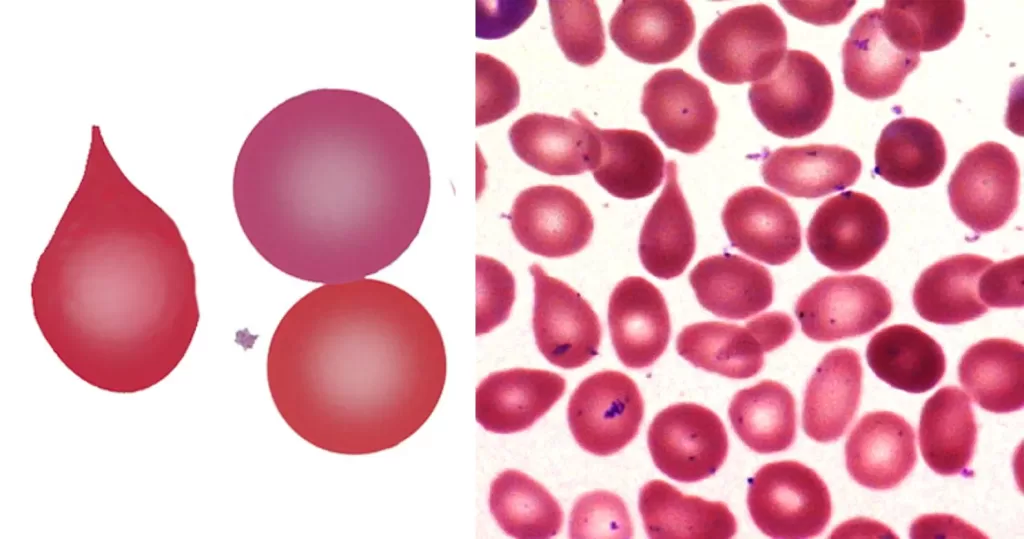
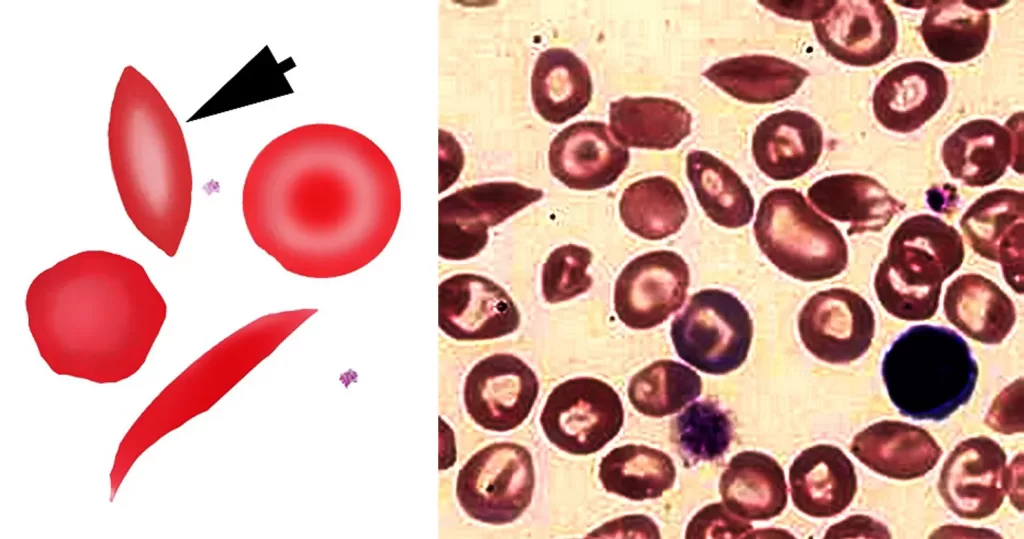
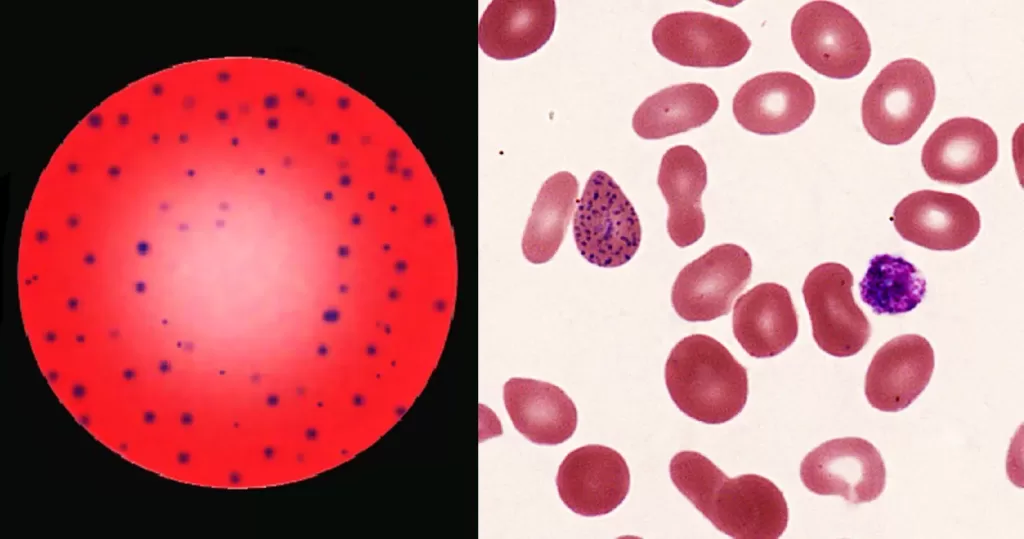
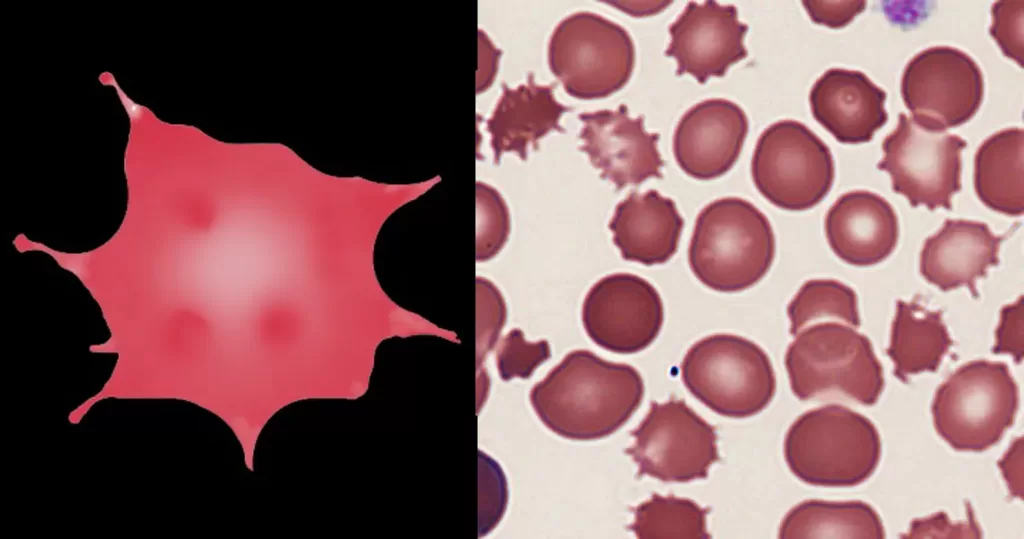
RBC (Red Blood Count)
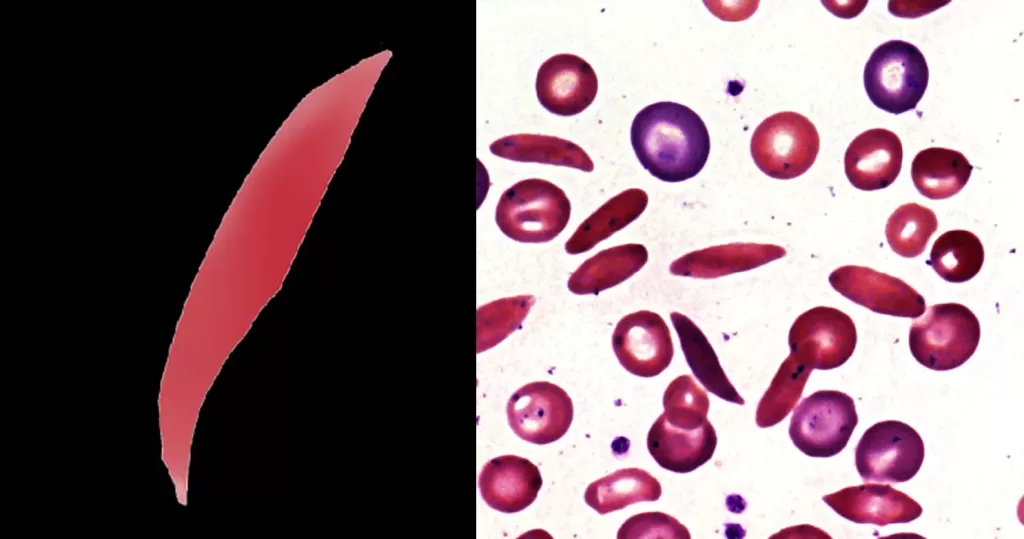
Hemoglobin (Hgb):
Hemoglobin is the amount of oxygen carrying protein contained within the red blood cells.
Hemoglobin Too High: Rule out lung disease, living
at high altitude, excessive bone marrow production of blood cells,
kidney tumors, hepatomas (liver tumors), uterine leiomyomas, cerebellar
hemangioblastomas, and sickle cell anemia.
Hemoglobin Too Low: Rule out anemia due to
nutritional deficiencies, blood loss, destruction of blood cells
internally, or failure to produce blood in the bone marrow.
Hematocrit (HCT, Packed Cell Volume or PCV):
The hematocrit is the percentage of the blood volume occupied by red
blood cells. Men have a slightly higher hematocrit percentages than
women because women lose a bit of blood each month during their
menstrual cycle.
Hematocrit Too High: Rule out smoking (due to too much carbon dioxide exposure), high altitude, chronic lung disease, and newborn syndrome.
Hematocrit Too Low: Rule out anemia due to
nutritional deficiencies, blood loss, and destruction of blood cells
internally, or failure to produce blood in the bone marrow.
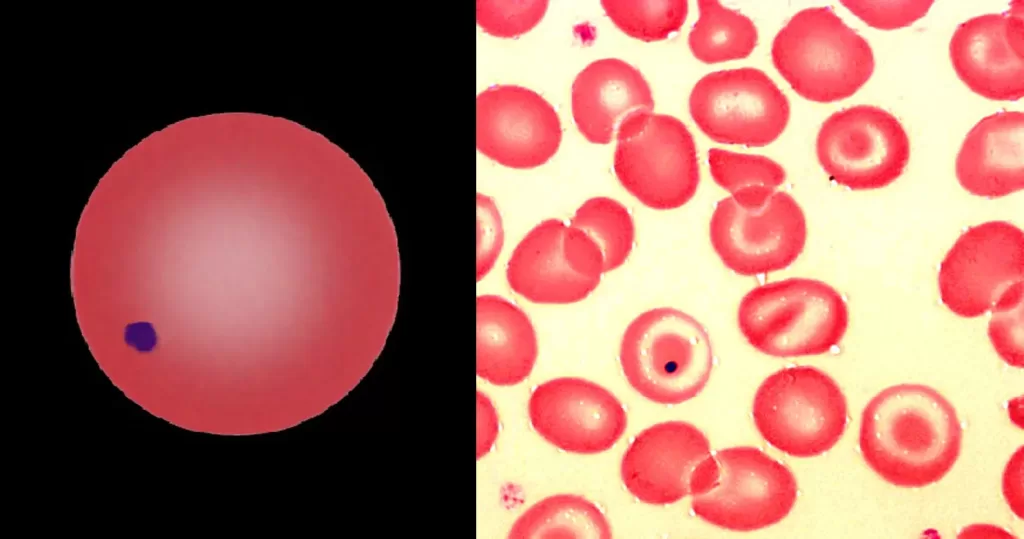
MCH (Mean Corpuscular Hemoglobin or Mean Corpuscular Volume (MCV):
MCH test helps diagnose the type of anemia.
MCH Too High: Rule out B12 deficiency, folate deficiency,
ineffective production in the bone marrow, or recent blood loss with
replacement by newer (and larger) reticulocytic cells from the bone
marrow, and in vitro or in vivo hemolysis.
MCH Too Low in the lab test: Rule out iron deficiency.
MCHC (Mean Corpuscular Hemoglobin Content or concentration):
MCHC denotes the volume and character of the hemoglobin and is the most accurate of the red cell indices.
MCHC Too High: Rule out spherocytosis (the cells are old and not being replaced as often), and in vitro or in vivo hemolysis.
MCHC Too Low: Rule out reticulocytes (too many young red cells), and iron deficiency.
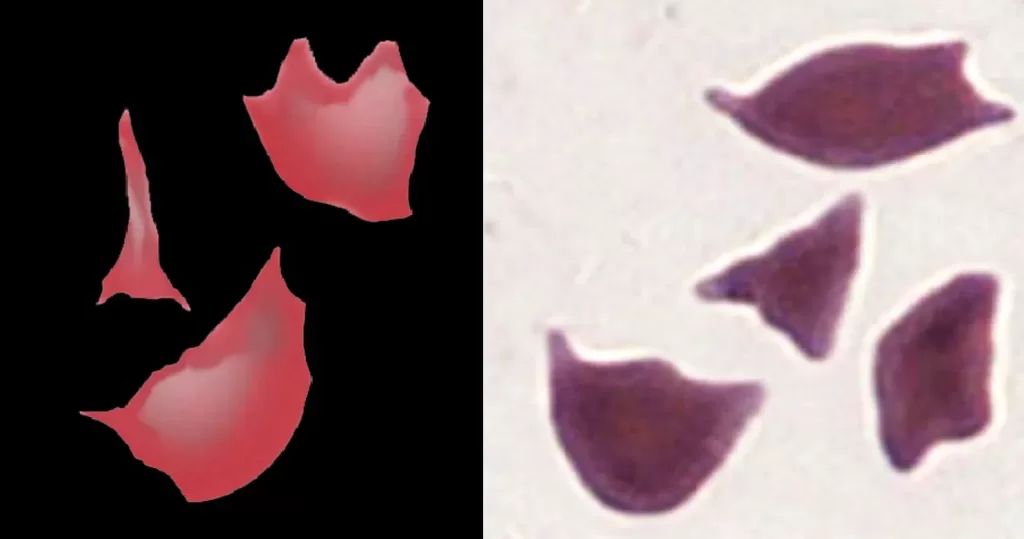
RDW (Red cell Distribution Width):
RDW test measures the different sizes and shapes of
the red cell. RDW is important because the more surface area the red
cell has, the better it can hook onto and transport oxygen through the
system.
RDW and MCV both Too High: Rule out liver disease, hemolytic anemia, Vitamin B12 deficiency, folic acid deficiency.
RDW Too High, but MCV Too Low: Rule out iron deficiency anemia, thalassemia intermedia (defective hemoglobin), fragmented cells.
RDW Too High, but MCV Normal: Rule out low Vitamin B12 or folic acid, iron deficiency anemia (early stages)
RDW Too Low: Rule out macrocytic
anemia (red cells are too large), microcytic anemia (red cells too
small). When the cells are all the same size, the RDW level will be low.
Note: One simple way to tell if you are anemic is to
look at your cheeks and chin in the mirror. If they look like they have
a blotchy tan, you are anemic and it will show up on a test within two
weeks. My recommendation is to take about 3/4 tea. blackstrap molasses
every day for a couple of months. When the anemia is gone, the tan will
be too. Read this article if you have this symptom: http://naturalhealthtechniques.com/SpecificDiseases/anemiatanchin.htm
Blood Gasses:
Blood gasses measure how much influence oxygen,
carbon dioxide and hydrogen ion concentration (pH) has on our body. This
lab test sample has to be taken from an artery to accurately measure the oxygen content. The other blood samples are taken from veins and both pH and CO2 can be measured using venous blood. Blood gas labtest results should be evaluated immediately.
Oxygen (PO2):
PO2 -The total oxygen concentration depends on total hemoglobin,
oxygen-carrying capability of hemoglobin, body temperature, blood pH,
certain blood enzymes and PO2 itself.
Oxygen lab test result Too High: Rule out gasses with high oxygen content (oxygen cages and anesthetic machines).
Oxygen Too Low (Hypoxia): Rule out respiratory disorders, heart shunts, or brain damage.
Carbon Dioxide (CO2):
CO2 level reflects the acid status of the blood and is a measure of the exchange of oxygen between the alveoli of the lungs.
Carbon Dioxide lab test result Too High: Rule out increased ventilation.
Carbon Dioxide Too Low: Rule out decreased
ventilation, increased acidity from uncontrolled diabetes, kidney
disease, heart shunts, and metabolic disorders.
Bicarbonate (HCO3):
Bicarbonate is maintained in health by conservation and production by
the renal tubules, so if there is kidney disease of some kind, the
values may be abnormal.
Cardiac Risk Factors
C Reactive Protein (CRP):
C Reactive Protein is a marker for inflammation.
C Reactive Protein lab test result Too High: Rule out inflammation in response to infection, vascular disease, heart attacks or strokes.
Homocysteine: Homocysteine is an amino acid that is
normally found in small amounts in the blood. Higher levels are
associated with increased risk of heart attack and other vascular
diseases. Men tend to have higher levels.
Homocysteine Too High:
Homocysteine levels rule out folic acid deficiency, Vitamin B12
deficiency, heredity, aging, kidney disease, and certain medications.
Lipoprotein or Lp:
Lipoproteins are a combination of water-soluble proteins containing
cholesterol and triglycerides and are present in the blood. The
lipoproteins in this test break the lipoprotein down into its alpha or
beta forms and determines the volumes of each. (Also see Cholesterol above).
Lipoproteins are also contained in the cholesterols high-density (HDL), low density (LDL), and very low density (VLDL)
lipoproteins which are all factors in heart disease and cholesterol
levels. These have been discussed under their individual cholesterol
categories above.
Lipoprotein lab test result Too High: Rule out
premature coronary heart disease (CHD) and the genetic link to heart
disease. Persons with diabetes and a high Lp level appear to have
increased risk of asymptomatic coronary disease.
Thyroid Lab Tests:
To evaluate the thyroid your doctor will take blood to run a Thyroid
Function Blood Panel, which will include many of the tests below
depending on the doctor?s education and the tests available at the
laboratory. It is important to understand each test because there is a
lot of confusion among doctors, nurses, lab
technicians, and patients as to which test is which. In particular, the
?Total T3″, ?Free T3″ and ?T3 Uptake tests? are very confusing, and are
not the same test.
You will want to have several thyroid factors evaluated from the following:
TSH (Thyroid Stimulating Hormone, sTSH):
The TSH test determines if your brain is producing the instructions for the body to respond by producing T4. Thyroid Stimulating Hormone is secreted by the pituitary gland and regulates the thyroid gland.
TSH Lab test results Too High: Rule out hypothyroidism.
TSH Lab test resultsToo Low: Rule out hyperthyroidism.
Total T4:
Total T4 measures the Free T4 and T4 bound to carrier proteins circulating within the blood.
Free T4 (Thyroxine, FT4):
Free T4 test is the basic thyroid molecule that circulates around the body before being activated to T3. The Free T4 directly
measures the free T4 in the blood. It is a more reliable, but a little
more expensive than Total T4. Some labs now do the Free T4 routinely
rather than the Total T4.
Free T4 Lab Test Too High: Rule out hyperthyroidism,
however technical artifact occurs when estrogen levels are higher from
pregnancy, birth control pills or estrogen replacement therapy.
Free Thyroxine Index (Free T4 Index, FTI or T7) :
Free Thyroxine Index is a mathematical computation
allows the lab to estimate the free thyroxine index from the T4 and T3
Uptake tests. The results tell us how much thyroid hormone is free in
the blood stream to work on the body. Unlike the T4 alone, it is not
affected by estrogen levels.
Total T3 (Triiodothyronine):
The Total T3 lab test is usually not ordered as a screening test, but
rather when thyroid disease is being evaluated. T3 is the more potent,
active, and shorter lived version of thyroid hormone. Some people with
high thyroid levels secrete more T3 than T4. In these hyperthyroid cases
the T4 can be normal, the T3 high, and the TSH low. The Total T3 reports the total amount of T3 in the bloodstream, including T3 bound to carrier proteins plus freely circulating T3.
Free T3 (Triiodothyronine):
The Free T3 lab test determines if the T4 is being
converted to its active form by the liver. This test measures the
free-floating T3 in the body.
T3 Resin Uptake or Thyroid Uptake.
The T3 Resin Uptake lab test confuses doctors, nurses, and patients. First, this is not
a thyroid test, but a test on the proteins that carry thyroid around in
your blood stream. Not only that, a high test number may indicate a low
level of the protein! The method of reporting varies from lab to lab.
The Resin T3 Uptake is used to assess the binding
capacity of the serum for thyroid hormone. The T3 Resin test is only
useful in conjunction with Total T4 or Total T3. If a patient has a high
total T4, it may be due to overproduction of thyroid hormone
(hyperthyroidism) or to an excess of one of the thyroid binding
proteins, usually Thyroid Binding Globulin (TBG). If the high Total T4
is secondary to high TBG, the Resin T3 will be low; otherwise it will be
normal or elevated. So, if the Total T4 or Total T3 deviates from
normal in one direction and the Resin T3 Uptake deviates in the opposite
direction, then the abnormality is due to changes in binding capacity.
If not, then it can be attributed to a true change in thyroid function
(i.e. hyperthyroidism or hypothyroidism). Estrogens increase the binding
capacity and decrease both the free labeled hormone and the Resin T3
uptake.
(Gee, I can see why it is so confusing!)
Thyroid Antibody test:
The thyroid antibody lab test is used to rule out autoimmune
hyperthyroidism diseases including Hashimoto?s disease (autoimmune
thyroiditis) and Graves? disease (toxic diffuse goiter).
Reverse T3 (the isomer of T3:
Reverse T3 (RT3) lab test is formed when T4 is deiodinated at the 5
position (T3 is formed from deiodination of the 5? position). RT3 has
little or no biological activity and serves as a disposal path for T4.
During periods of starvation or severe physical stress, the level of RT3
increases while the level of T3 decreases. In hypothyroidism both RT3
and T3 levels decrease. Thus RT3 can be used to help distinguish between
hypothyroidism and the changes in thyroid function associated with
acute illness (Euthyroid Sick Syndrome).
Cortisol:
Cortisol levels are tested to see how you are handling stress. Stress suppresses the thyroid.
Copper Levels:
Copper levels are run to rule out Wilson?s Disease and heavy metal interference. Copper
inhibits TRH (Thyroid Releasing Hormone) at the hypothalamus and in the
case of Wilson?s Syndrome, builds up in the liver preventing conversion
of T4 to T3. TRH is the messenger that keeps track of how much and
which thyroid hormones are needed.
Note: To read more about thyroid function, the role of iodine, and how to establish health using natural methods go to: http://naturalhealthtechniques.com/SpecificDiseases/thyroid_disease.htm
LAB TESTS FOR DIABETES AND BLOOD SUGAR MANAGEMENT:
Blood Glucose curve:
The blood glucose curve is created by a series of blood glucose lab
tests taken by either drawing blood out of a pre-inserted catheter or by
sticking the finger with a lancet at many different time intervals,
usually within a 1-3 day period. The goal is to figure out how many
units of insulin are needed to maintain the proper blood glucose levels
in the patient.
Glucose:
Glucose is a measure of the sugar level in the blood. The normal
range for a fasting glucose is 60 -109 mg/dl. According the 1999
American Dietetic Association criteria, diabetes is diagnosed with
fasting plasma glucose levels of 126 or more. A precursor, Impaired Fasting Glucose (IFG) is defined as a fasting glucose of 110 ? 125 mg/dl. Sometimes a glucose tolerance test,
which involves giving you a sugary drink followed by several blood
glucose tests, is necessary to properly sort out normal from IFG from
diabetes. Variations in lab normals exist.
Europeans tend to use a 2-hour after eating definition of diabetes
rather than a fasting glucose. Using the European standards tends to
increase the number of people who are classified as having diabetes. To
differentiate persistent problems from transient ones, a second blood
glucose sample should be taken within 24 hours.
Glucose Lab test Too High (Hyperglycemia): Rule out
eating before the test, IV glucose, diabetes, glucocorticoids,
thiazides, pheochromocytoma, Cushing?s syndrome, acromegaly, brain
damage, liver disease, nephrosis, hyperadrenocorticism,
hyperglucagonemia, ammonia toxicosis (cattle), milk fever (cattle),
insulin dosage too small, hyperthyroidism, pain induced catecholamine
and glucocorticoid release, listeriosis (sheep), transport tetany
(sheep), and pancreatitis.
Glucose Too Low (Hypoglycemia): Rule out Addison?s
disease (adrenocortical insufficiency), myxedema, aflatoxicosis (a
disease in horses where they eat too much grain infected with molds),
too much exercise, glycogen storage diseases, gram-negative septicemia,
liver insufficiency or failure, hyperinsulinism from insulin overdose or
insulinoma, hypopituitarism, juvenile hypoglycemia (toy and miniature
dog breeds), ketosis (cattle), malabsorption, neonatal hypoglycemia,
cancers, pregnancy toxemia (sheep), starvation, and malabsorption.
Glycohemoglobin (Hemoglobin A1 or A1C, HbA1C):
Glycohemoglobin measures the amount of glucose chemically attached to
your red blood cells. Since blood cells live about 3 months, it tells
us your average glucose for the last 6 ? 8 weeks. A high level suggests
poor diabetes control.
Insulin-Like Growth Factor I (IGF-1):
The IGF-1 lab test is used to determine acromegaly,
in which somatomedin-C (Sm-C) and growth factor (GH) are increased. It
is also used to evaluate hypopituitarism. Sm-C is a polypeptide hormone
produced by the liver and other tissues, with effects on growth
promoting activity and glucose metabolism (insulin-like activity). Sm-C
is carried in blood bound to a carrier protein, which prolongs its
half-life. Its level is therefore more constant than that of growth
hormone.
IGF-1 Too Low: Rule out ageing, hypopituitarism,
malnutrition, diabetes mellitus, Laron dwarfism, hypothyroidism,
maternal deprivation syndrome, pubertal delay, cirrhosis,
hepatoma, nonfunctioning pituitary tumors with constitutional
delay of growth, and anorexia nervosa.
IGF-1 Too High: Rule out adolescence, true
precocious puberty, pregnancy, obesity, pituitary gigantism, acromegaly
and diabetic retinopathy. Since Sm-C is decreased with malnutrition, its
concentration provides an index with which to monitor therapy for food
deprivation.
Insulin:
Insulin is secreted by the pancreas in response to eating or elevated
blood sugar. Insulin levels vary widely from person to person depending
upon an individual?s insulin sensitivity (or conversely, their insulin
resistance) and when the last meal occurred. Insulin, when measured by
itself, at random times, is rarely useful.
Insulin Lab Test Too Low: Rule out diabetes. Insulin is deficient in persons with Type 1 diabetes (insulin-dependent diabetes), and borderline deficient in persons with Type 2 diabetes. The natural evolution of Type 2 diabetes causes insulin levels to fall from high levels to low levels over a course of years.
Insulin Too much: Rule out hypoglycemia.
HOMA-IR (the Homeostasis Model of Insulin Resistance):
HOMA-IR is a measure of insulin. Insulin resistance
is a risk factor for coronary disease so assessing an individual?s
insulin resistance may have some value. Other diseases associated with
an increased HOMA-IR test are AIDS and polycystic ovary syndrome (PCOS).
Polycystic ovary women have insulin resistance independent of obesity.
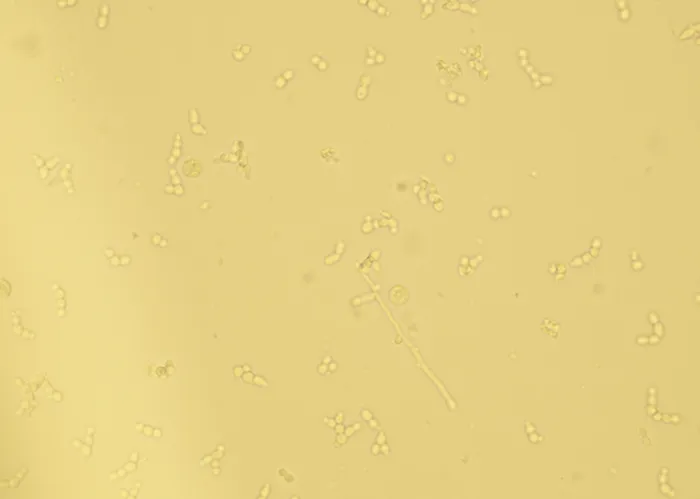
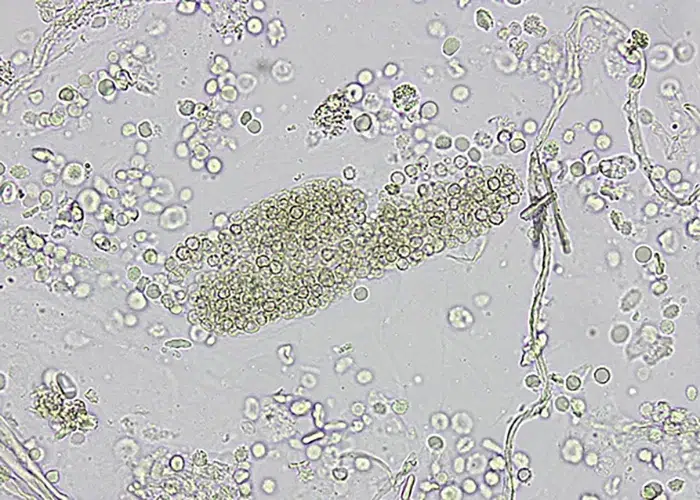
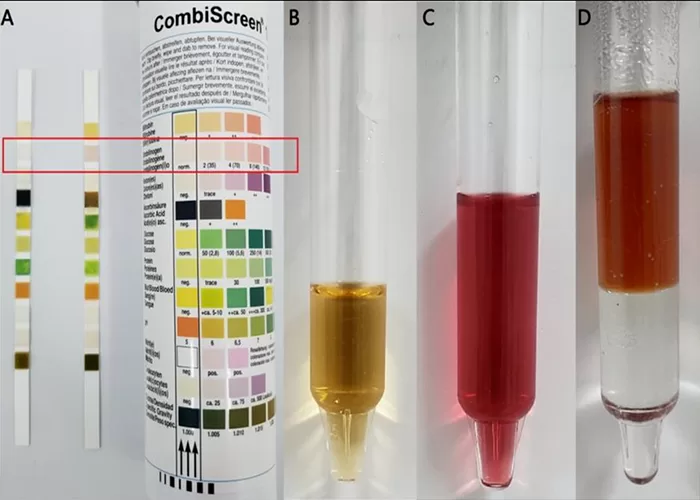
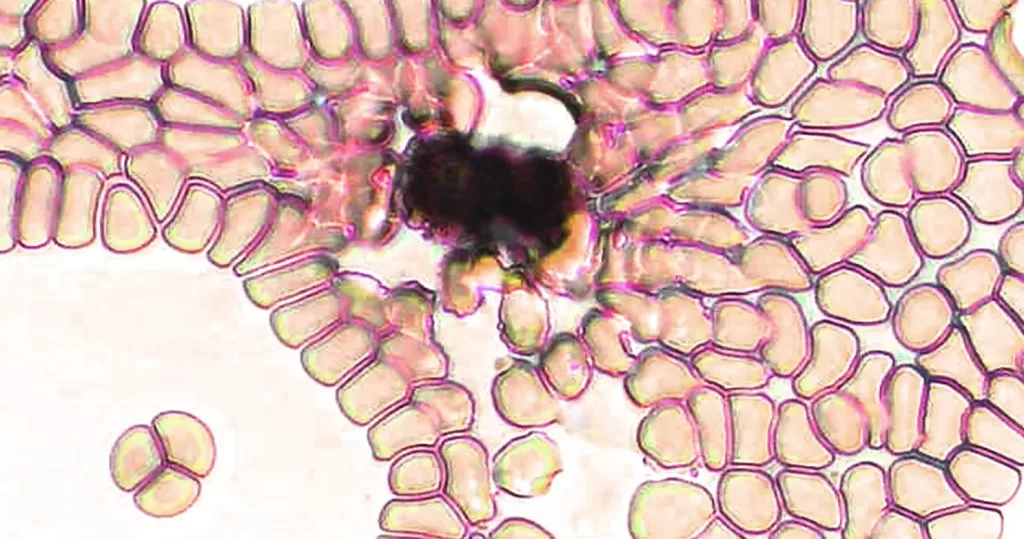
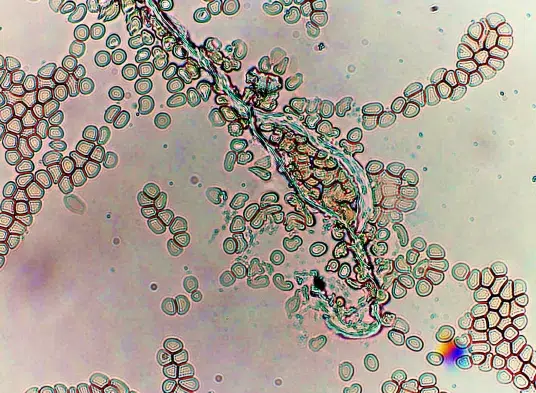
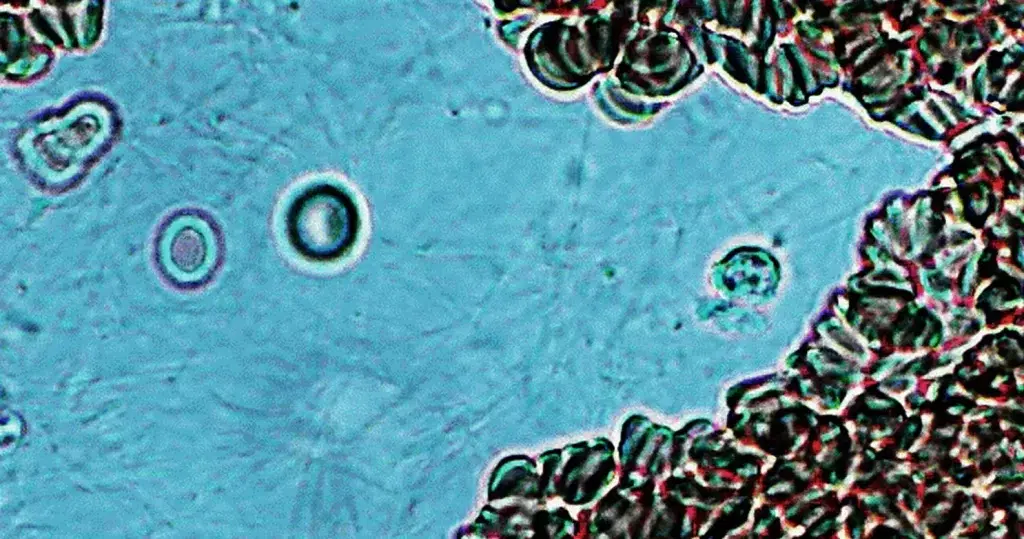
THE URINALYSIS:
The urinalysis lab test measures the presence and
amount of a number of chemicals in the urine, which reflect much about
the health of the kidneys, along with cells that may be present in the
urine (for example, red blood cells, white blood cells, or groups of
these called ?casts?). Also, the lab looks for crystals, bacteria, and
other organisms in the urinary sediment. Each of these elements give
hints as to function of the kidneys, kidney tubules, ureters (small
tubes that connect the kidneys with the urinary bladder), and the
urinary bladder.
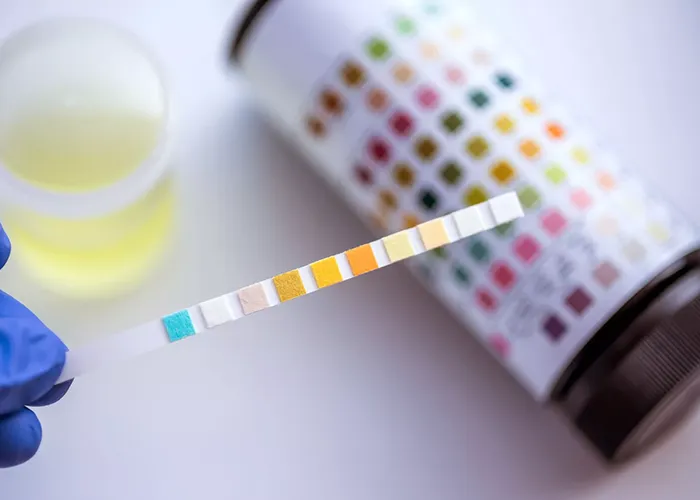
Urine lab tests are typically evaluated with a reagent strip that is
briefly dipped into the urine sample. The technician reads the colors of
each test and compares them with a reference chart. The urine is then
spun down and the sediment checked for cells, yeast, bacteria, crystals,
and casts (groups of dead cells that indicate kidney tubule damage).
For a more in depth interpretation with pictures go to: http://naturalhealthtechniques.com/urinalysis-interpretation.htm
Here are some tips on collecting the urine sample for lab tests:
If you are doing a free-catch sample, it is nice to
have some urine caught in the beginning, middle and end of the urination
process. Why? The first fraction coming out flushes cells, yeast and
bacteria from the vulva or prepuce areas and the urethra (the tube that
connects the bladder to the outside world). The middle fraction is a
better picture of what has been stored in the bladder. The tail-end of
the sample gives a better idea of how the kidneys look.
My personal choice as a veterinarian is to stick a long needle
directly into the bladder so I don?t have to guess if the bacteria,
yeast and dead cells are from the urethra or the bladder. It doesn?t
hurt much and helps alleviate contamination of the sample. That way I
can treat the core cause instead of a secondary infection of some type.
Medical doctors sometimes insert a catheter into the bladder for this
reason.
If you are trying to get a sample from your pet at home, one easy way
to do it is to tape a small cup to the bottom of the ruler. As the pet
urinates, you can slip the cup underneath them without leaning over and
startling them. Label the sample with the date and time it was collected
then get the sample to your vet right away for lab testing.
Urine Volume:
Increased (Polyuria): Rule out acute renal disease,
chronic renal disease, diabetes mellitus hepatic failure,
hyperadrenocorticism, hypercalcemia, hyperparathyroidism (cats and
humans), nephrogenic diabetes insipidus, pituitary diabetes insipidus,
postobstructive diuresis, primary renal glycosuria, psychogenic
polydipsia, pyelonephritis, and pyometra.
Decreased (Oliguria): Rule out acute renal failure, dehydration, shock, terminal chronic renal disease, and urinary tract obstruction.
pH :
pH is a measure of hydrogen ion concentration
(acidity or alkalinity) of the urine. Fresh samples are necessary for
an accurate lab test reading because urine becomes alkaline when it is
older because the carbon dioxide escapes and the bacteria in the urine
convert urea to ammonia which is very alkaline. The healthy, normal pH
of human urine is less than 7.
Too High (Alkaline): Rule out diets high in vegetables and urinary tract infections (the bacteria convert the urine to ammonia). Note: This is the only instance where I tell people to eat lots of protein and junk food for 2-3 days!
Too Low (Acid): Rule out diets high in protein and refined carbohydrates, anorexia, and starvation.
Specific Gravity (SG):
Specific Gravity measures how dilute your urine is.
Specific gravity takes into account the weight of the urine and particle
size. Water would have a specific gravity of 1.000 Most human urine is
around 1.010, but it can vary greatly depending on when you drank fluids
last, or if you are dehydrated.
Glucose in the urine:
Normally there is no glucose in urine.
Detectable Glucose (Glucosuria): Rule out diabetes,
kidney disease (decreased tubular reabsorption), acromegaly,
hyperpituitarism, bovine milk fever, bovine neurologic disease,
excessive insulin dosage, fear or exertional catacholamine release,
Fanconi-like syndrome, moribund animals, sheep endotoxemia, and drugs
such as ACTH, glucocorticoids, fluids, ketamine, morphine,
phenothiazine, and xylazine. A small number of people have glucose in
their urine with normal blood glucose levels, however any glucose in the
urine would raise the possibility of diabetes or glucose intolerance.
Protein in the Urine:
Protein (Proteinuria): When you urinate and see foam
in the toilet bowl, this can indicate either sugar or protein and is
not normal. A urinalysis and blood work are used to determine what the
problem is. Talk with your doctor if you see this. Normally there is no
protein detectable on a urinalysis strip.
Detectable Protein: Rule out kidney damage,
increased glomerular permeability (from fever, cardiac disease, central
nervous system disease, shock, muscular exertion), blood in the urine,
inflammation, cancers, infection. High concentrations of very small
proteins can also show up in the urine such as Bence Jones protein,
hemoglobin monomers, and myoglobin. Up to 10% of children can have
protein in their urine. Sometimes this is due to colostral antibodies.
Certain diseases require the use of a special, more sensitive (and more expensive) test for protein called a microalbumin test. A microalbumin test is very useful in screening for early damage to the kidneys from diabetes.
False Positive causes: Rule out urine too alkaline.
Blood in the Urine:
Blood (Hematuria): Normally there is no blood in the urine lab test.
Detectable Blood: Rule out infection, kidney stones,
trauma, and bleeding from bladder or kidney tumors. The technician may
indicate whether the blood is hemolyzed (dissolved blood) or
non-hemolyzed (intact red blood cells). Note that blood also occurs when
a woman is having her period or in the dog when she is in heat so it
can be normal. Ask more questions if you see blood in the urine.
False Positive causes: Rarely, muscle injury can
cause myoglobin to appear in the urine which also causes the reagent pad
to falsely indicate blood. Mensus in humans or animals in
heat will also have blood in their urine as a normal occurrence.
Bilirubin in the Urine:
Bilirubin (Bilirubinuria): Normally there is no bilirubin or urobilinogen in the urine. These are pigments that are cleared by the liver.
Detectable Bilirubin: Rule out liver or gallbladder
disease, obstruction of bile flow, intravascular hemolysis,
hemoglobinuria, and tubular cell conjugation of free bilirubin.
False positives: Urine color may interfere with the reading of this lab test.
Nitrate:
Normally negative, the presence of nitrates usually indicates a
urinary tract infection caused from nitrate reducing bacteria including
veillonellae, haemophili, staphylococci, corynebacteria, lactobacilli,
flavobacteria and fusobacteria.
Leukocytes (Leukocyte esterase):
Normally negative. Leukocytes are the white blood cells (or pus cells).
Detectable Leukocytes: Rule out urinary tract infection.
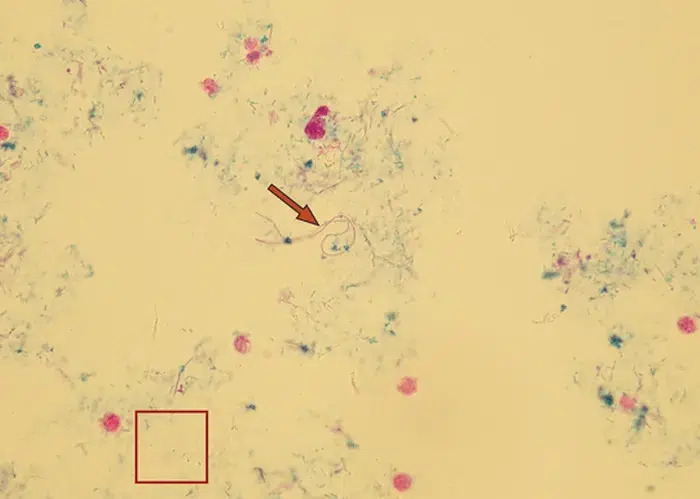
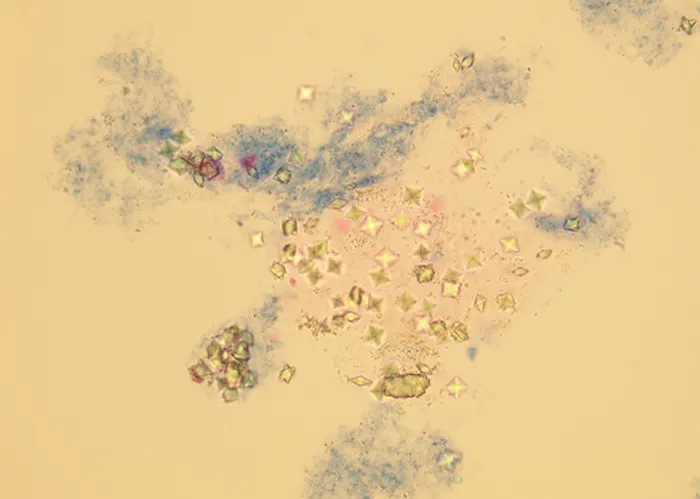
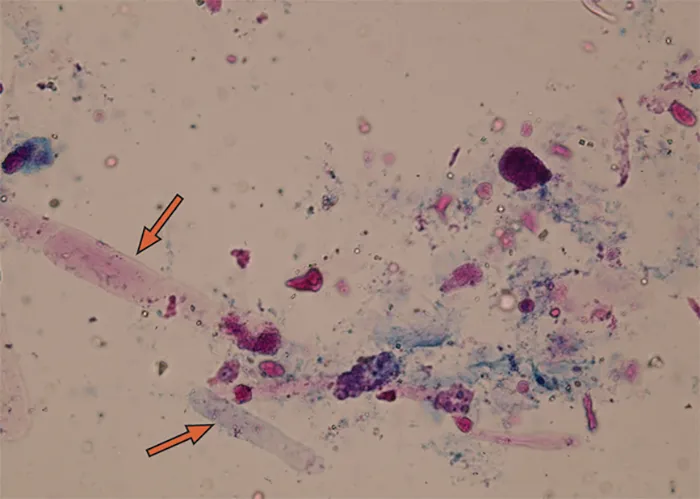
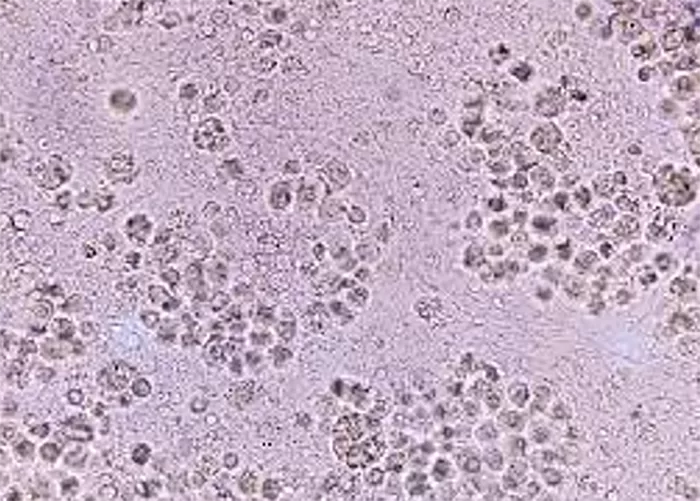
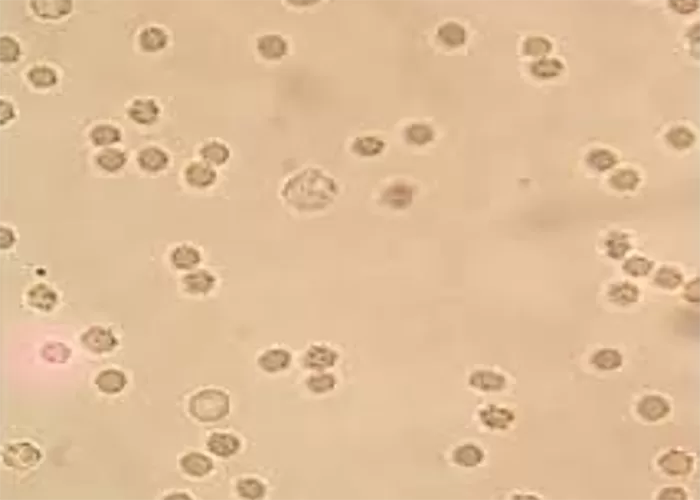
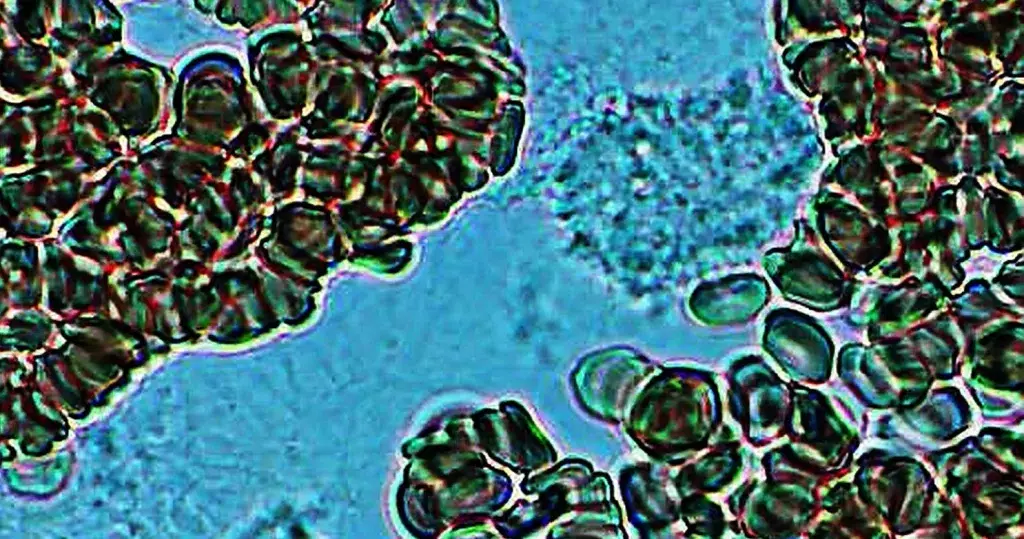
Sediment in the Urine:
Sediment: Here the doctor, nurse, or lab technician
looks under a microscope at a portion of your urine that has been spun
in a centrifuge. Items such as mucous and squamous cells are commonly
seen. Abnormal findings would include more than 0-2 red blood cells,
more than 0-2 white blood cells, crystals, casts, renal tubular cells,
yeast or bacteria. (Bacteria and yeast can be present if there was
contamination at the time of collection.). The pH of the urine
determines what types of crystals will be formed.
For LOTS more info on urine sediments see the following handout: http://naturalhealthtechniques.com/SpecificDiseases/bladder_kidney_stones.htm
Sex Hormone Profile Lab Tests:
Sex hormone tests are popular these days and can be done at home via a
saliva or urine test or done in a doctor?s office using blood.
Estrogen:
Estrogen is tested to evaluate menstrual status and
sexual maturity. Estrogens are responsible for proliferation and growth
of specific cells and are responsible for development of most secondary
sexual characteristics in the female. Three types of estrogens are present in significant quantities in the blood lab test, estradiol, estrone, and estriol.
Estrogens Too High: Rule out gynecomastia (feminization syndrome) and estrogen-influenced ovarian tumors.
Estradiol:
Estradiol is the most common type of estrogen and the most important
estrogen in evaluating the fertility of the female because it is
produced almost solely by the ovary. In women estradiol varies according
to age, normal menstrual cycles, taking birth control pills or estrogen
replacement.
Estriol (E3):
Estriol is the major estrogen in the pregnant female produced by the
placenta. Excretion of estriol increases around the eighth week of
gestation and continues to rise until shortly before delivery. Serial
urine and blood studies of this hormone are used to assess placental
function and fetal normality in high-risk pregnancies. Falling values
during pregnancy suggest fetoplacental deterioration and require prompt
reassessment of the pregnancy, including the possibility of early
delivery.
Progesterone:
Progesterone is produced in the ovaries during the
second half of the menstrual cycle, by the placenta during pregnancy,
and in small amounts from the adrenal glands and testes. Progesterone
prepares the uterus for implantation of the fetus and is responsible for
increasing breast milk in preparation for lactation. This is
another important hormone to evaluate for evaluating fertility in the
female.
After ovulation, an increase of progesterone causes the uterine
lining to thicken in preparation for the implantation of a fertilized
egg. If this event does not take place, progesterone and estrogen levels
fall, resulting in shedding of the uterine lining. Progesterone is
essential during pregnancy, not only ensuring normal functioning of the
placenta, but passing into the developing baby?s circulation, where it
is converted in the adrenal glands to corticosteroid hormones.
Testosterone:
Testosterone is the most important of the male sex
hormones. It is responsible for stimulating bone and muscle growth, and
sexual development. It is produced by the testes and in very small
amounts by the ovaries in women. Most testosterone tests measure total
testosterone. Testosterone stimulates sperm production
(spermatogenesis), and influences the development of male secondary sex
characteristics.
Testosterone Too High: Overproduction of
testosterone caused by testicular, adrenal, or pituitary tumors in the
young male may result in precocious (early) puberty. Overproduction of
testosterone in females, caused by ovarian and adrenal tumors, can
result in masculinization, the symptoms of which include cessation of
the menstrual cycle (amenorrhea) and excessive growth of body hair
(hirsutism).
Testosterone Too Low: When reduced levels of
testosterone in the male indicate under activity of the testes
(hypogonadism), testosterone stimulation tests may be ordered.
Tests for Sexually Transmitted Diseases:
Herpes Serology
(Herpes simplex viruses, HSV): A blood lab test for
herpes is now available. A blood test only tells whether you have been
infected with the herpes virus. Herpes serology cannot tell when you
became infected, what body parts will be affected, whether you will
develop symptoms of herpes or if your symptoms are due to herpes. A swab
of an active lesion is the only way to detect the virus itself. It may
take between six and eight weeks to detect antibodies in a herpes blood
test after first becoming infected with HSV. Also, antibodies may
disappear with time, especially if the person has infrequent recurrences
of herpes breakouts.
Genital Herpes is caused by either Herpes Simplex Virus type I (HSV-1) or Herpes Simplex Virus type II (HSV-2).
Herpes Simplex Virus II (HSV-2) is the usual cause of repeated attacks
of genital herpes and HSV-1 is usually the type that is responsible for
cold sores (oral herpes).
False positives and negatives: All lab tests
occasionally give incorrect results. The herpes test can be falsely
positive 5% of the time and a false negative result 15% of the time?so
before a marital blow-out happens?repeat the test using a different lab.
Note: I don?t know about the vaginal herpes, but the oral herpes usually goes away when you stop ?holding your tongue?.
So speak your truth and those cold sores should disappear in 1-3 days. I
have seen this as an effective treatment MANY times. Oh, and many more
people than you could imagine are infected with the vaginal herpes, so
if you are single, don?t let that keep you single for life. The truth
shall set you free. Forgive yourself and move on. Just be discerning
about whom you talk to about it and don?t have sex with those that are
unaware you have it. There are drugs and homeopathic drops that help
control active outbreaks.
Frequently Asked Questions about Lab Test Results:
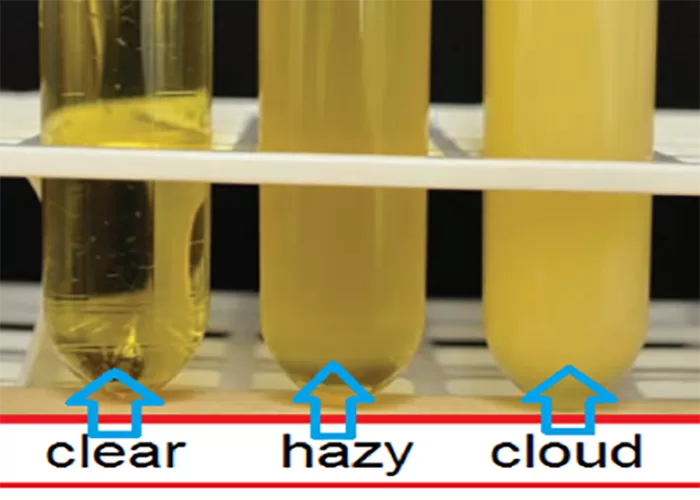
Why do I have to have an empty stomach for at least 12 hours before they draw my blood for the lab tests? When
we eat, fat gets into our bloodstream and can affect the tests giving
false positive or false negative results. Fat in the bloodstream gives
cloudy serum and the scientific instruments they use to test different
blood levels can?t see through the cloudiness.
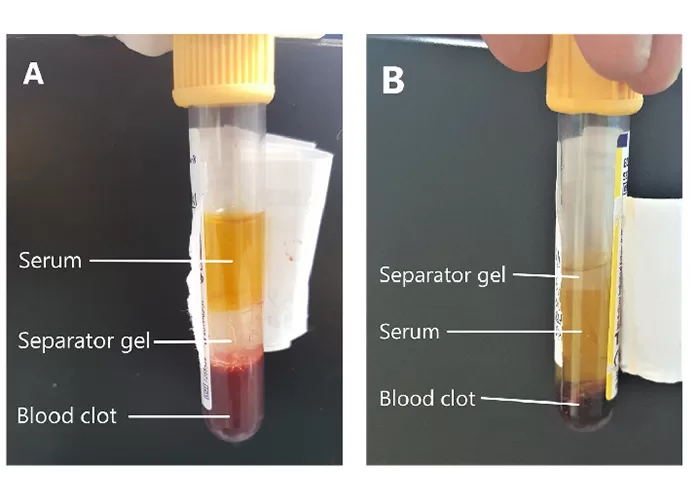
Why do they put the blood in several tubes each with a different color at the top of the tube? Each
tube your sample is put in does something different to the sample. Some
have preservatives in them, some have anticoagulants, and some don?t
have anything. Preservatives can prevent the breakdown of certain
enzymes so that the blood can be stored until it gets to the lab to be
tested. Anticoagulants prevent the blood from clotting so cells can be
counted and looked at with lab equipment. When the tube doesn?t have
anything in it (the red top tubes) we want the blood to clot so we can
gather the serum and not the red or white cells. This way we can run
different blood tests to see all aspects of how your body is functioning
or not functioning.
Helpful Links and References for Lab Test Results:
- Veterinary Laboratory Medicine Clinical Pathology, 2nd Edition by J. Robert Duncan, DVM, Ph.D. and Keither W. Prasse, DVM, Ph.D.
- What is a Rule Out? http://naturalhealthtechniques.com/whats-a-rule-out.htm
- The Urinalysis Lab Test:
? 2005-2012 by Dr. Denice M. Moffat
For educational use
Contact Us:
only. Permission to make copies by you for you and your friends is
granted. If you find this site to be of value, a donation of any kind or
amount would be greatly appreciated. Some donation ideas include
signing up for our newsletter, making an appointment, a referral,
linking to the site from your site on an appropriate page and sending
money or a prayer are all acceptable donations of energy. I believe we
need to support those things that nourish us in any way if we’d like to
see them around in the future! You are encouraged to consult a
knowledgeable practitioner before utilizing any of the information in
this site. I am available for telephone consultations only at this
point. I love working on my site and hope that you get enjoyment and
healing from it. Namaste. Dr. Denice Moffat
Dr. Denice Moffat
1069 Elk Meadow Lane
Deary, Idaho 83823 U.S.A.
(208) 877-1222 Pacific Time (General Questions)
(208) 877-1969 Our dedicated Phone Consultation Line for Client Consults
Email Me**********************
http://naturalhealthtechniques.com/basicsofhealthlab_result_meaning1.htm Blood and Urine
Best Medical Intuitive Online