Differential Count
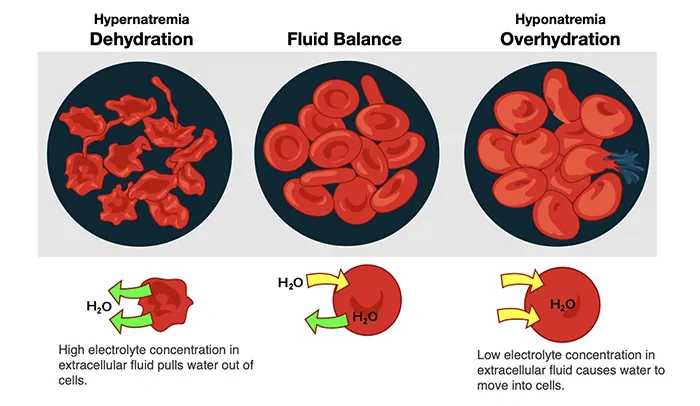
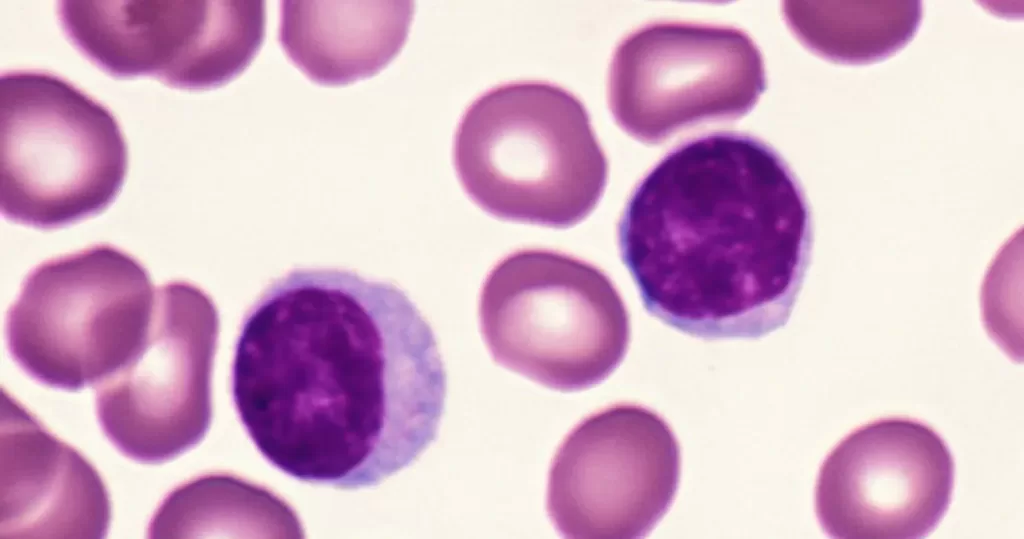
Leukocytes, also known as white blood cells (leukocytes), are nucleated cells found in the blood and lymphatic system, playing a central role in the body’s immune response. Leukocytes circulate in the bloodstream and are capable of migrating to tissues in response to various immune signals, where they participate in inflammatory and immune responses.
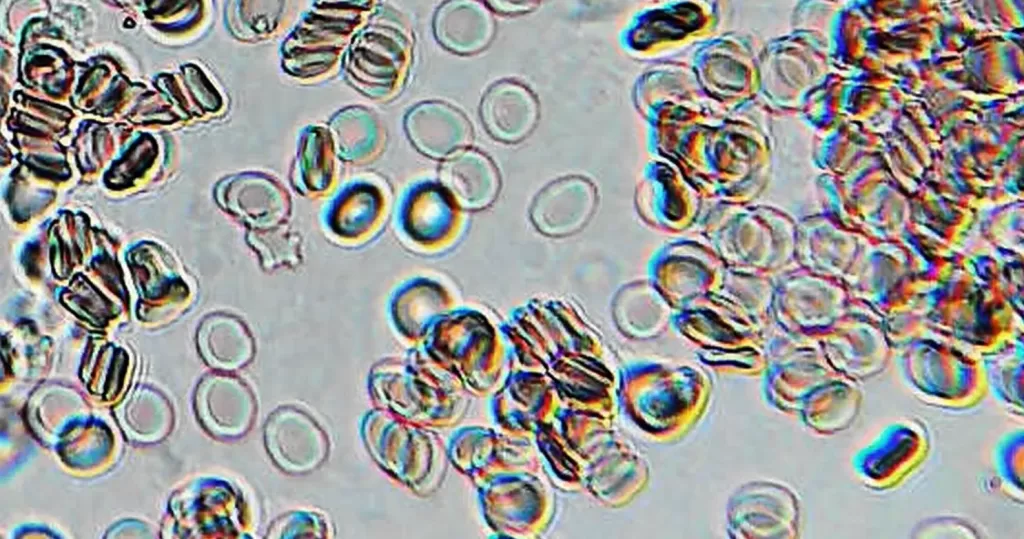
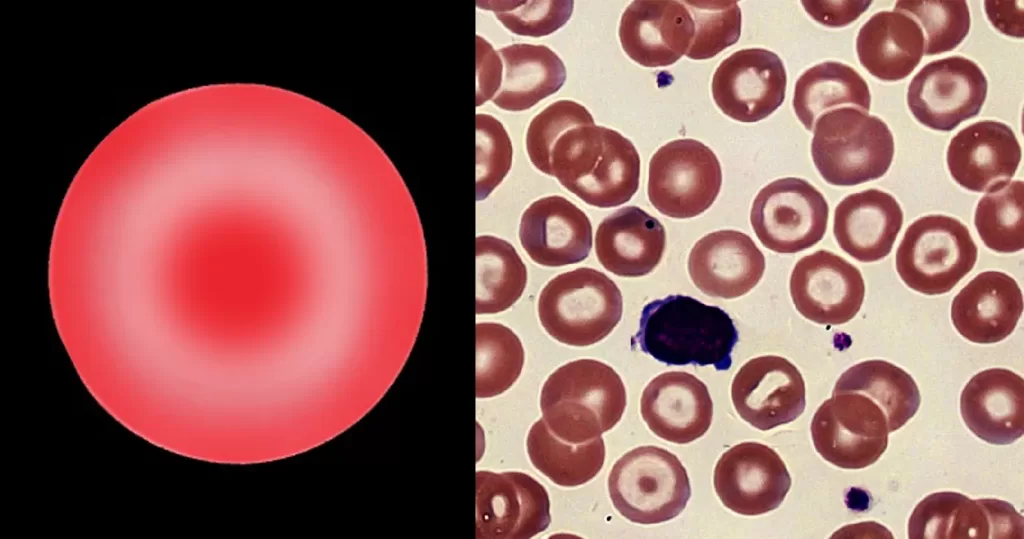
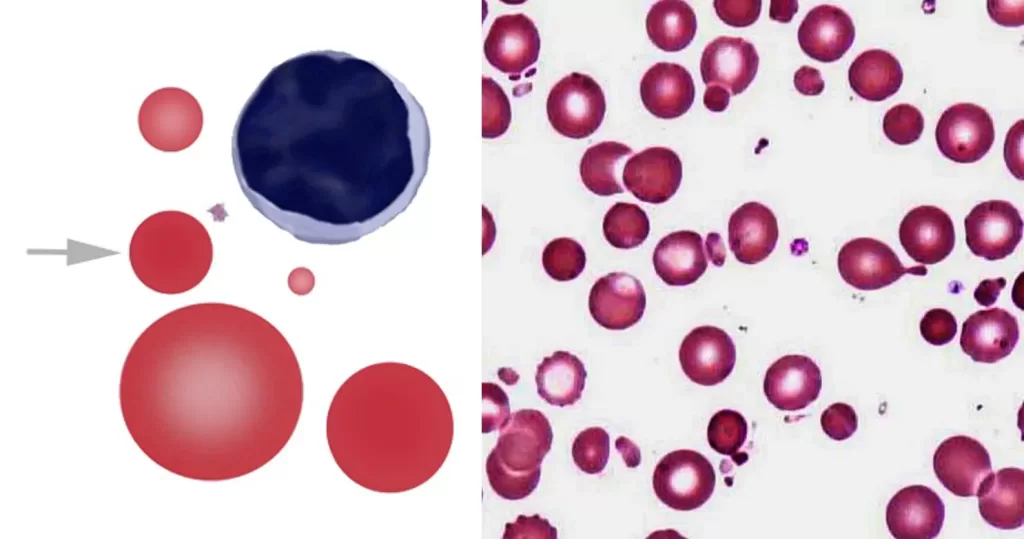
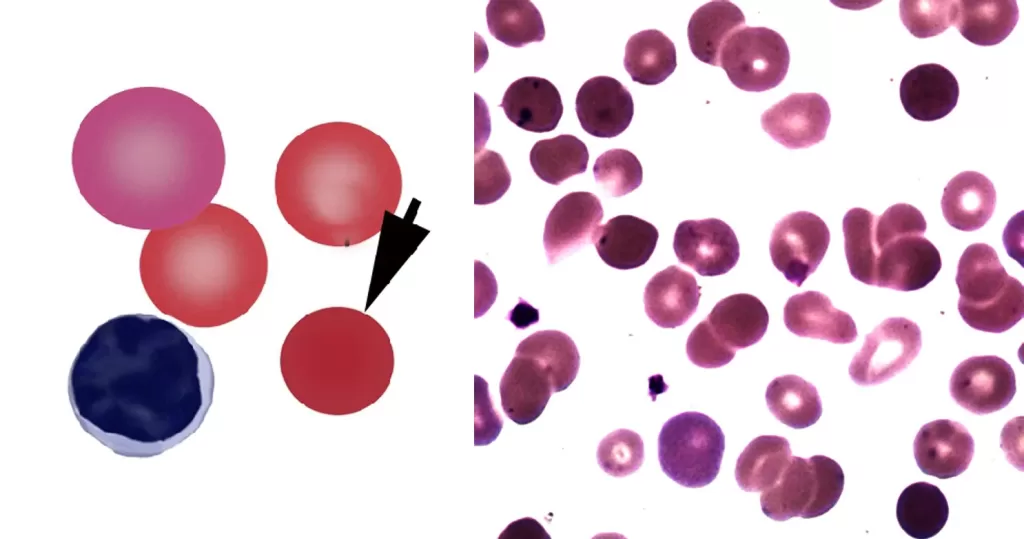
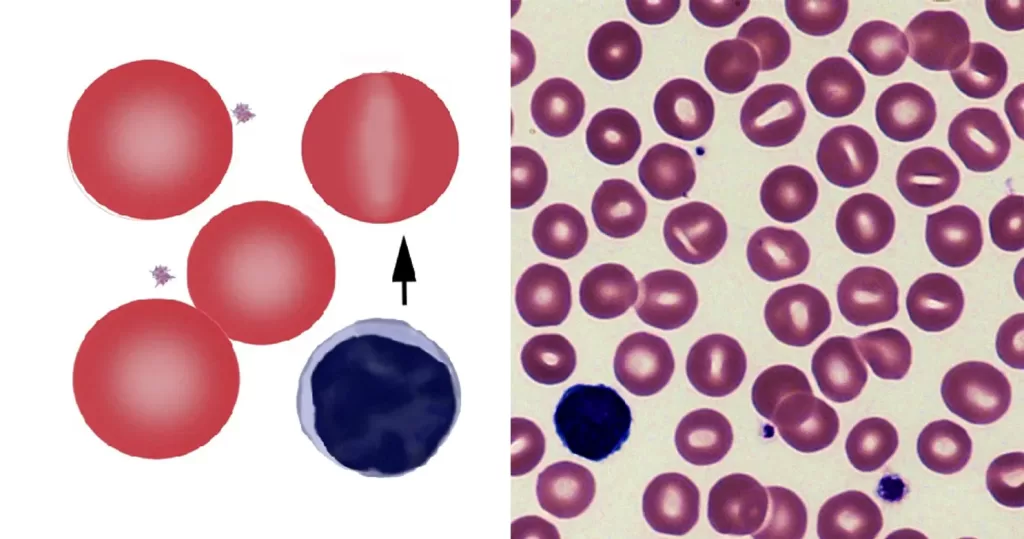
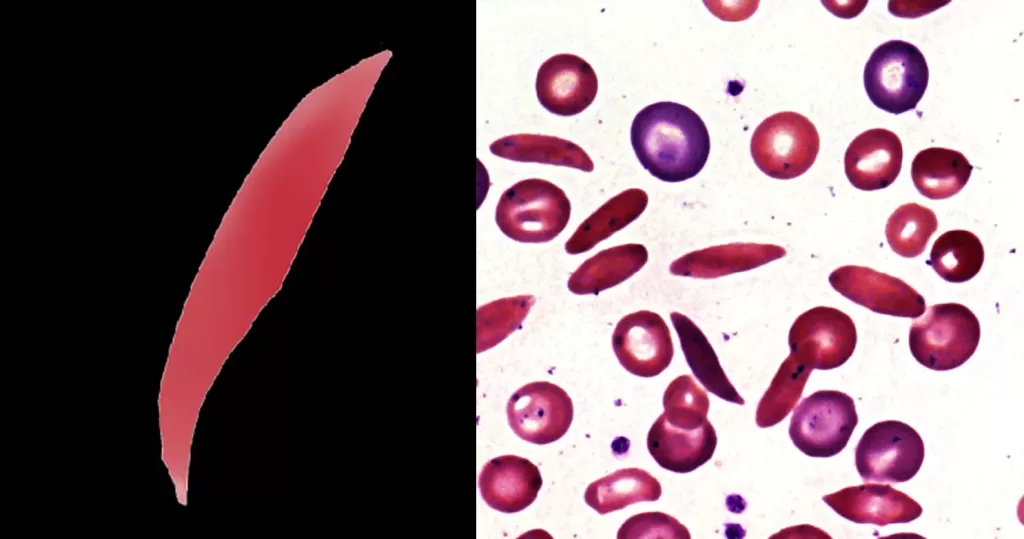
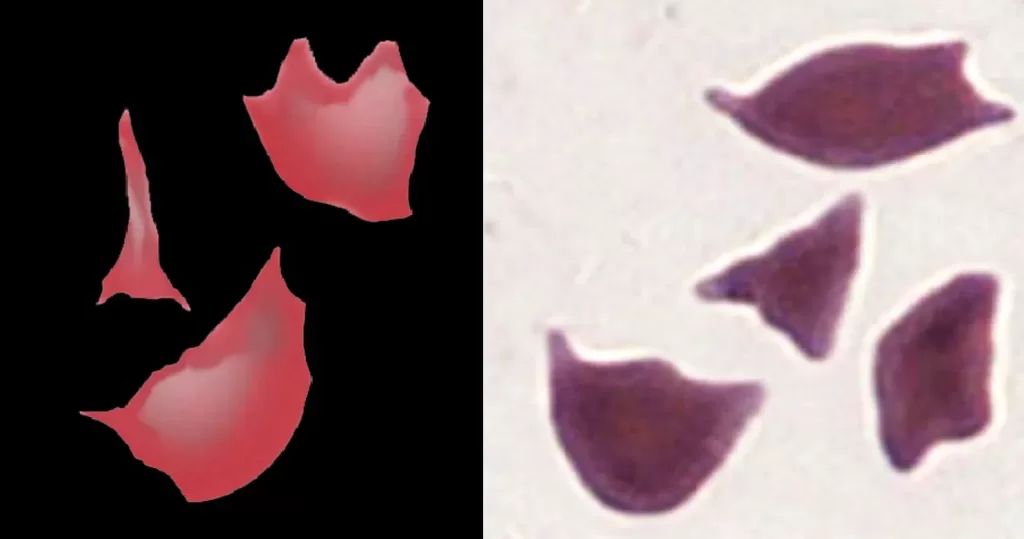
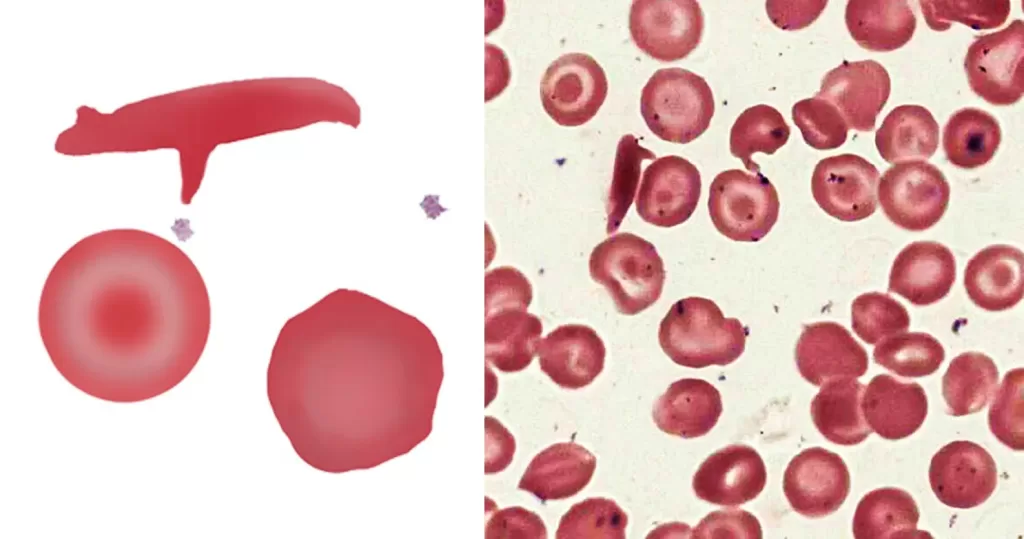
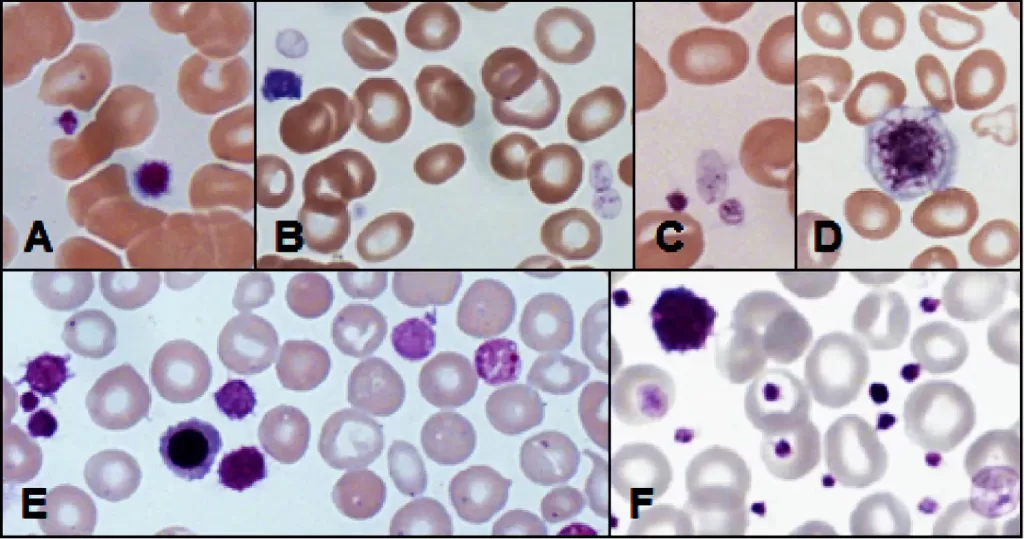
A differential leukocytes count is a laboratory test used to measure the relative proportions of the different types of leukocytes in a sample of peripheral blood. This test involves counting and classifying the various leukocytes subtypes that are classified into two major groups based on their appearance under microscope which are:
Granulocytes: These contain visible granules in their cytoplasm and include:
- Neutrophils: The most abundant type, responsible for phagocytosing (engulfing) and digesting pathogens, especially bacteria.
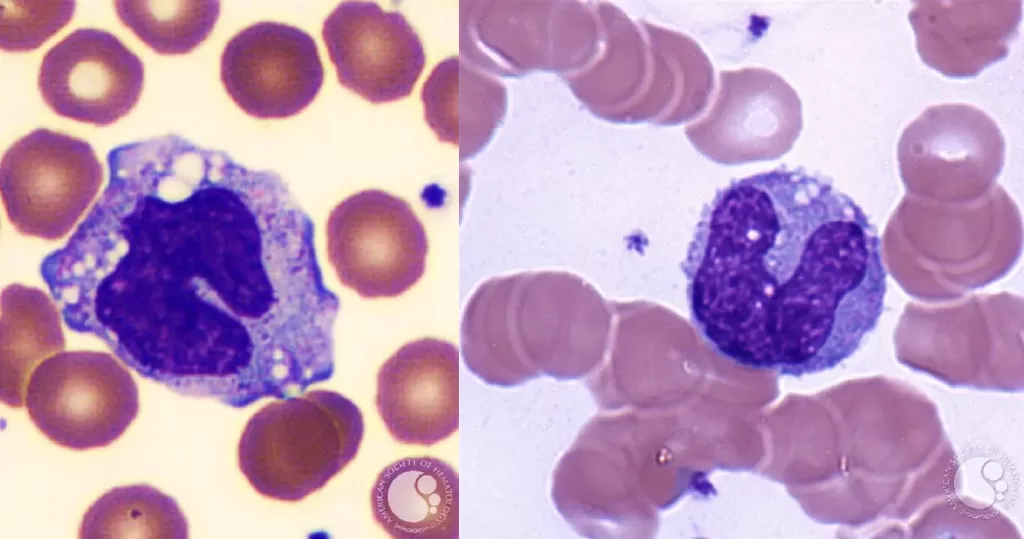
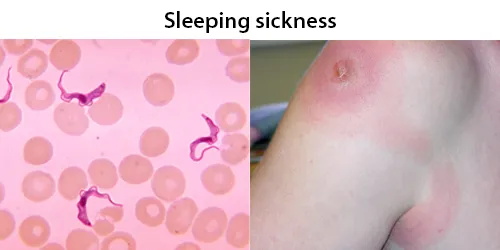
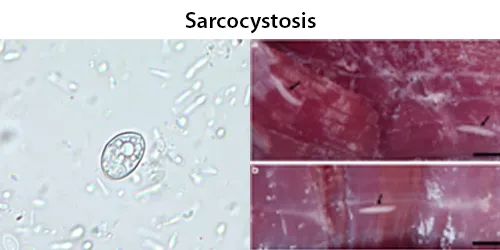
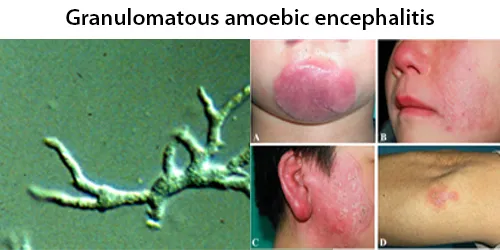
- Eosinophils: Primarily involved in fighting parasitic infections and modulating allergic responses.
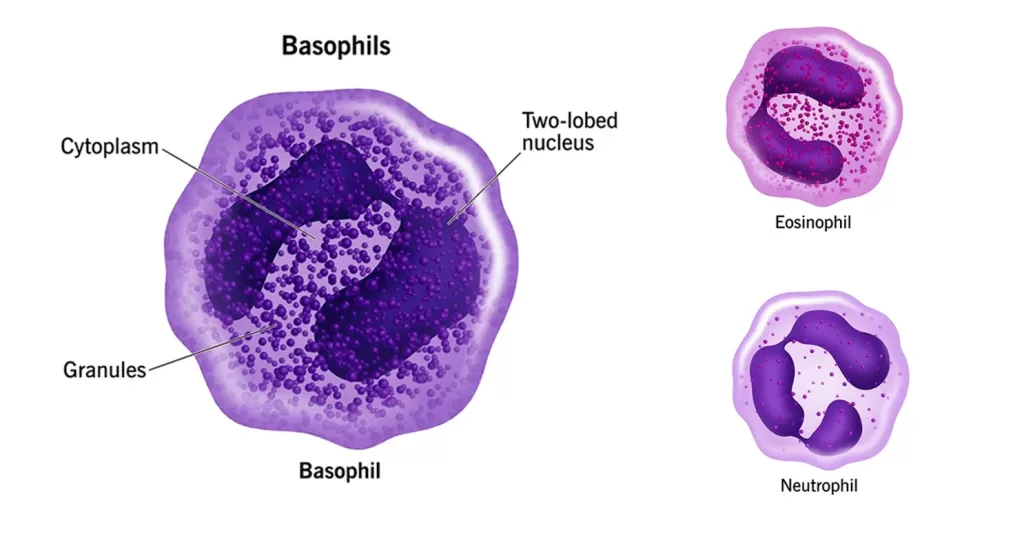
- Basophils: Release histamine and other mediators in allergic reactions and inflammation.
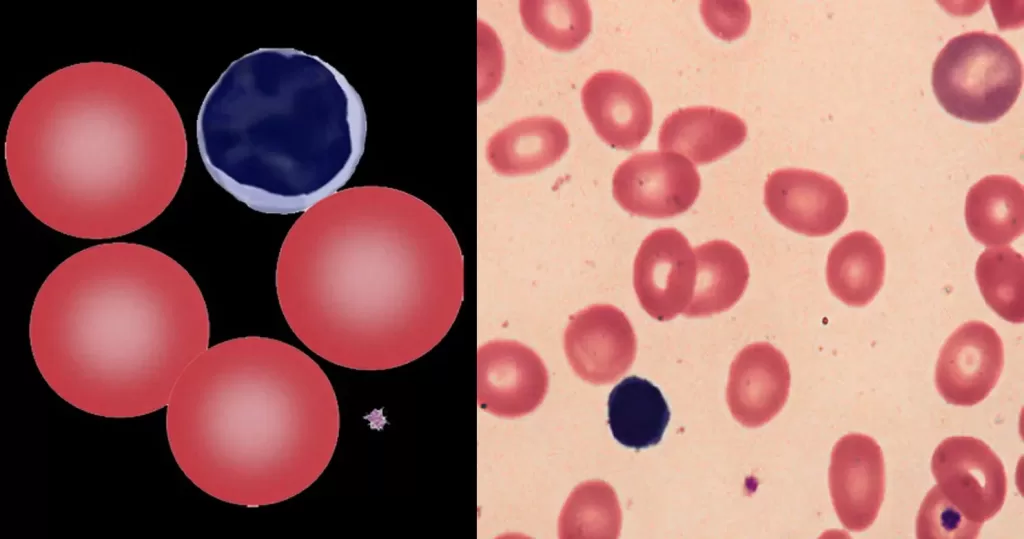
Agranulocytes: These lack visible granules in their cytoplasm and include:
- Lymphocytes: Key players in adaptive immunity, subdivided into:
- T cells: Involved in cell-mediated immunity (helping to destroy infected or cancerous cells).
- B cells: Produce antibodies to neutralize pathogens.
- Natural Killer (NK) cells: Part of the innate immune system, they target and destroy
infected or cancerous cells.
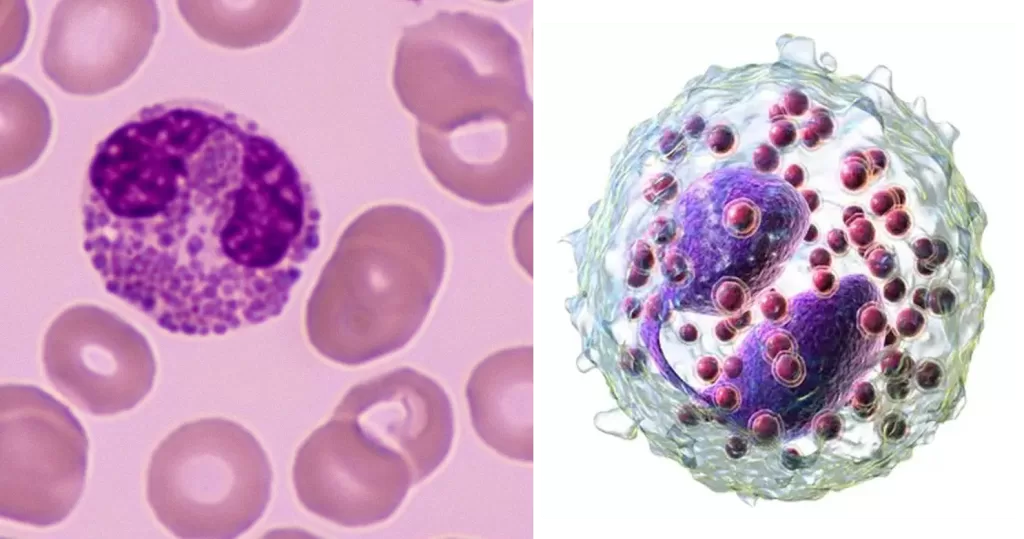
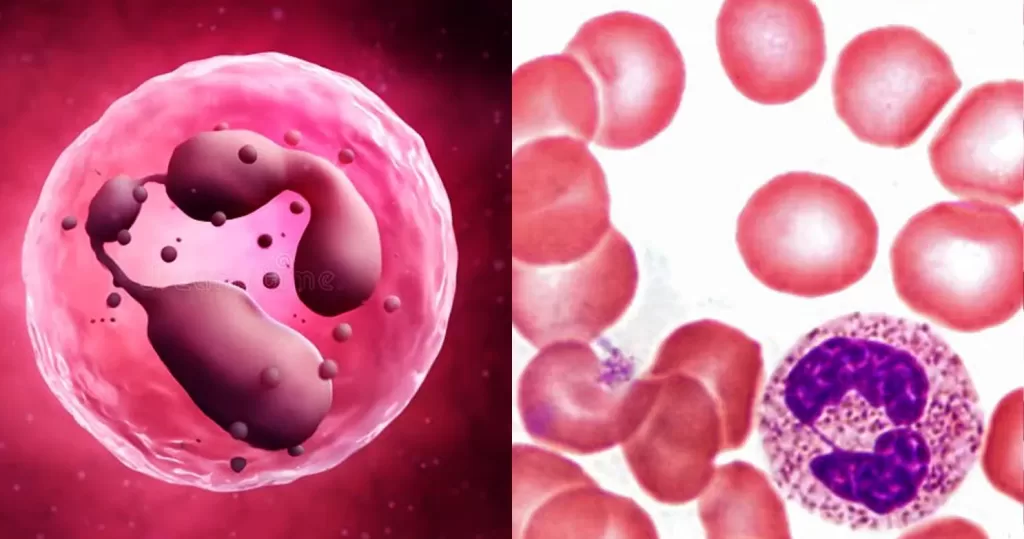
- Monocytes: The largest leukocytess, they differentiate into macrophages and dendritic cells, which are essential for phagocytosis and antigen presentation.
The distribution and absolute numbers of these cells can provide valuable diagnostic information regarding a wide range of physiological and pathological conditions, such as infections, inflammations, allergies, hematologic disorders, and immune system abnormalities. The differential count is often expressed as both a percentage of the total leukocytes population and an absolute count per unit of blood volume.
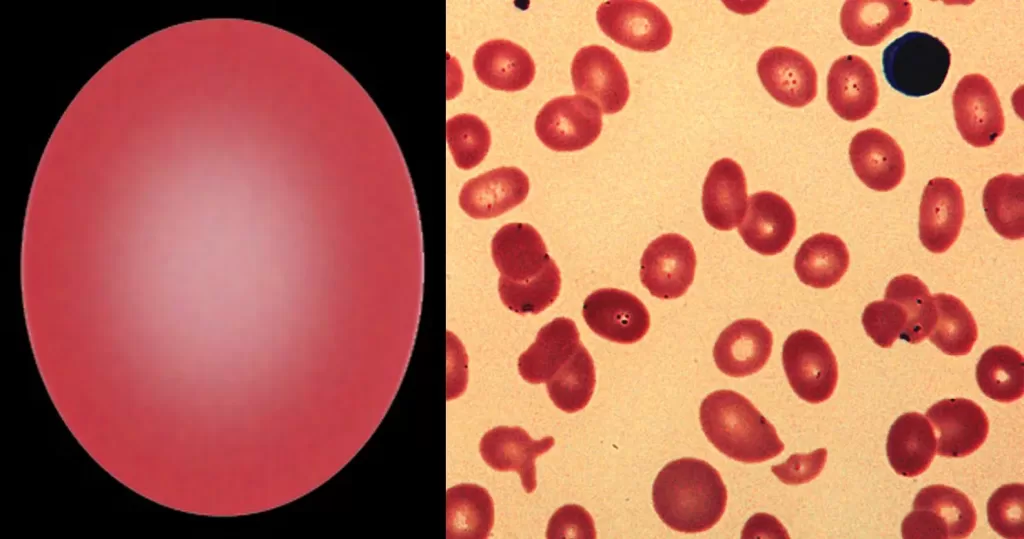
Performing a differential leukocytes count in a laboratory setting typically involves the following steps:
- Preparation of Blood Smear:
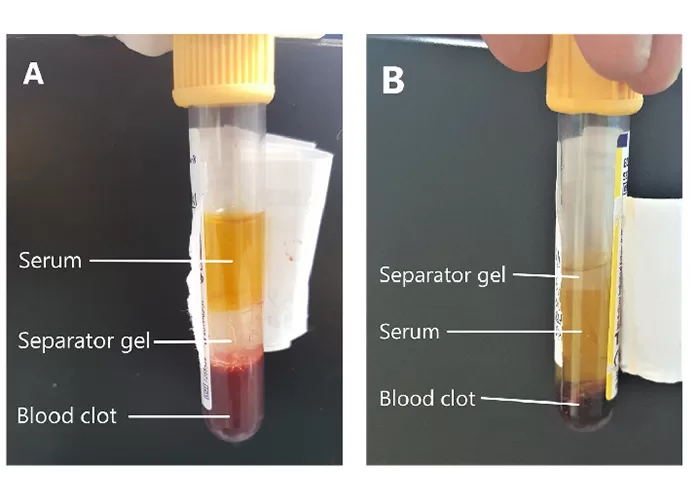
Obtain a Blood Sample: A blood sample is drawn from the patient, usually using a venipuncture method.
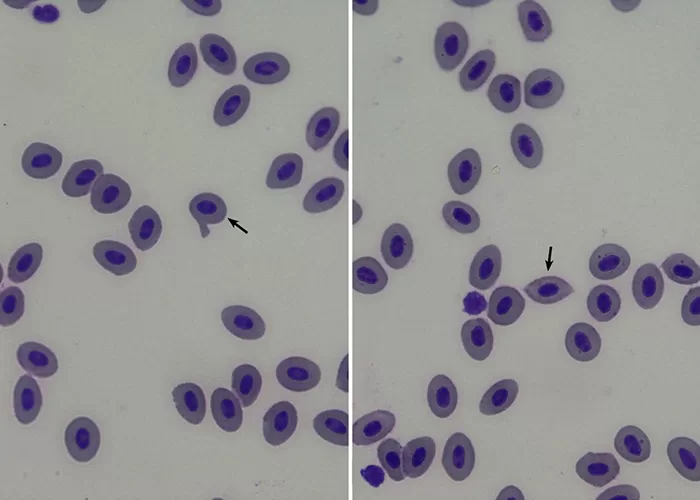
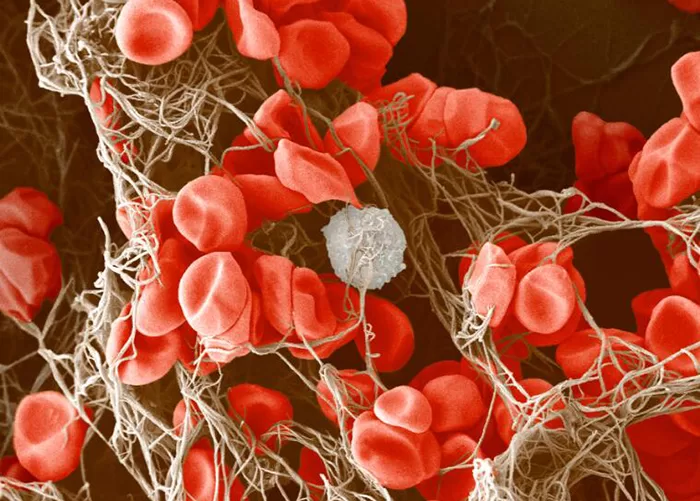
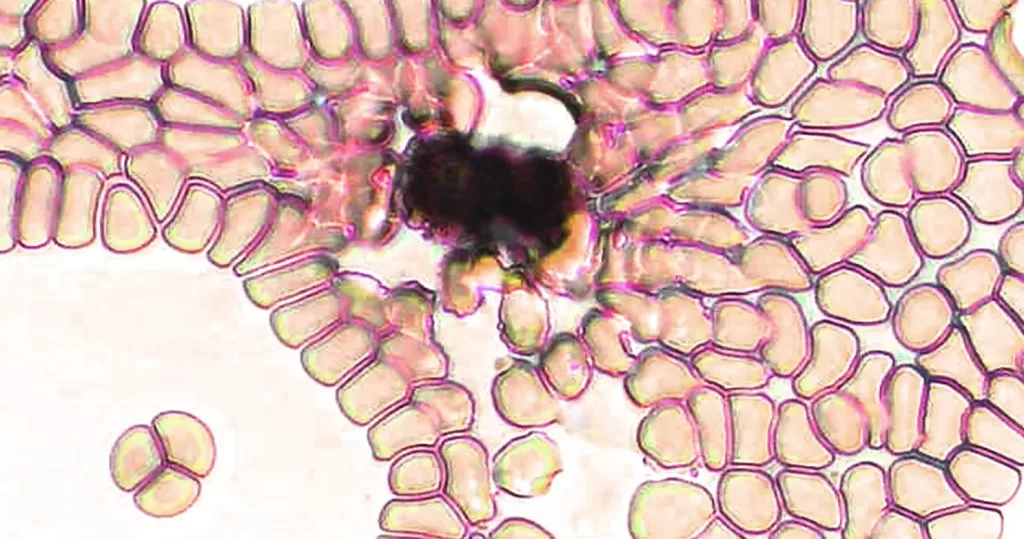
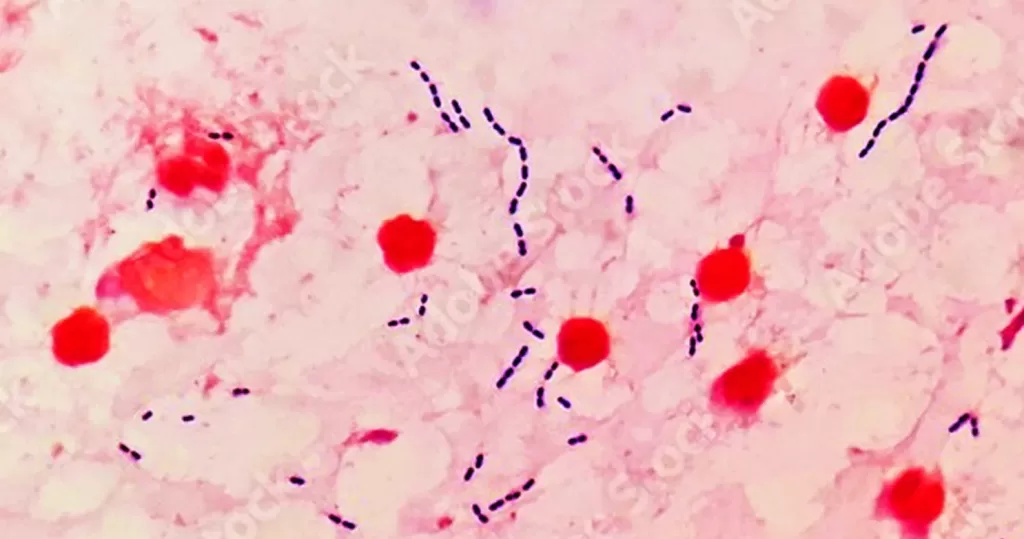
Prepare a Blood Smear: A drop of blood is placed on a clean glass microscope slide. A second slide is used to spread the blood drop evenly across the surface of the slide in a thin layer, creating a “feathered edge” where cells can be easily examined. - Staining the Slide:
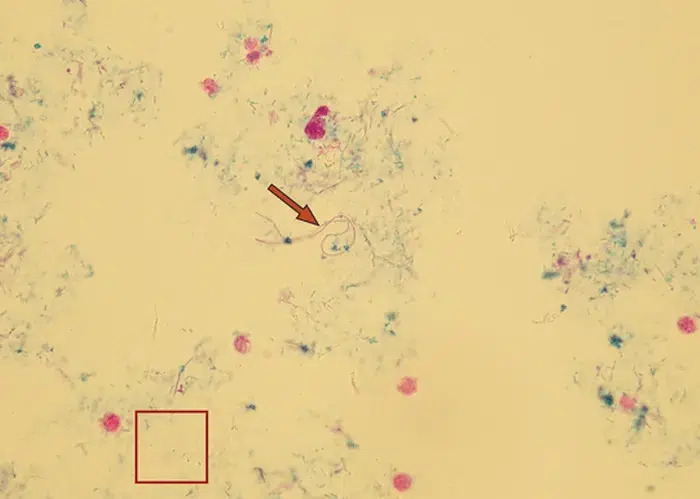
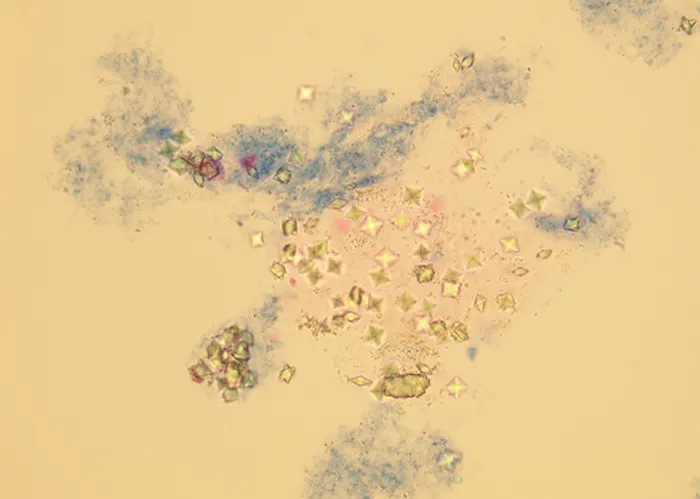
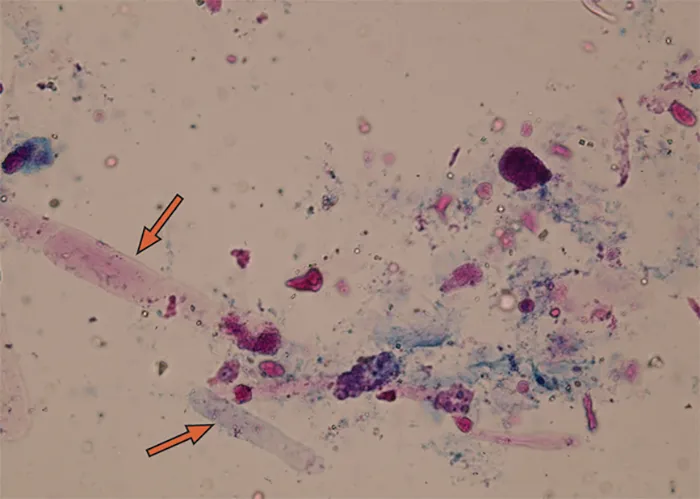
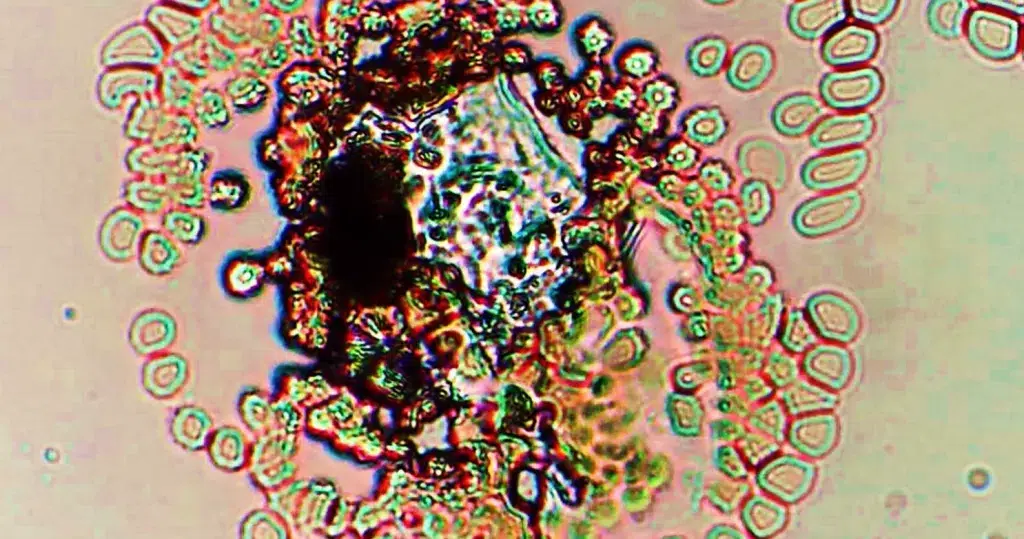
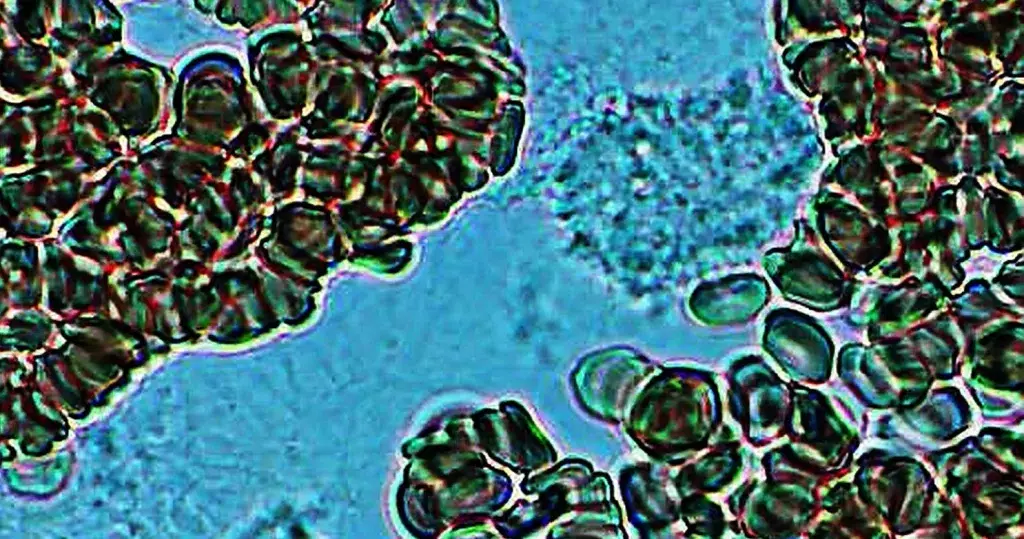
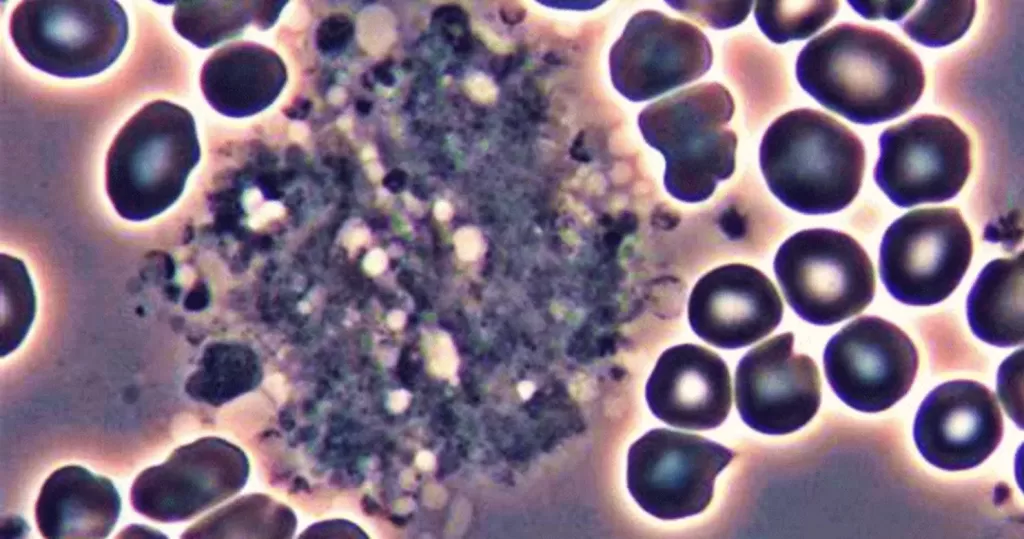
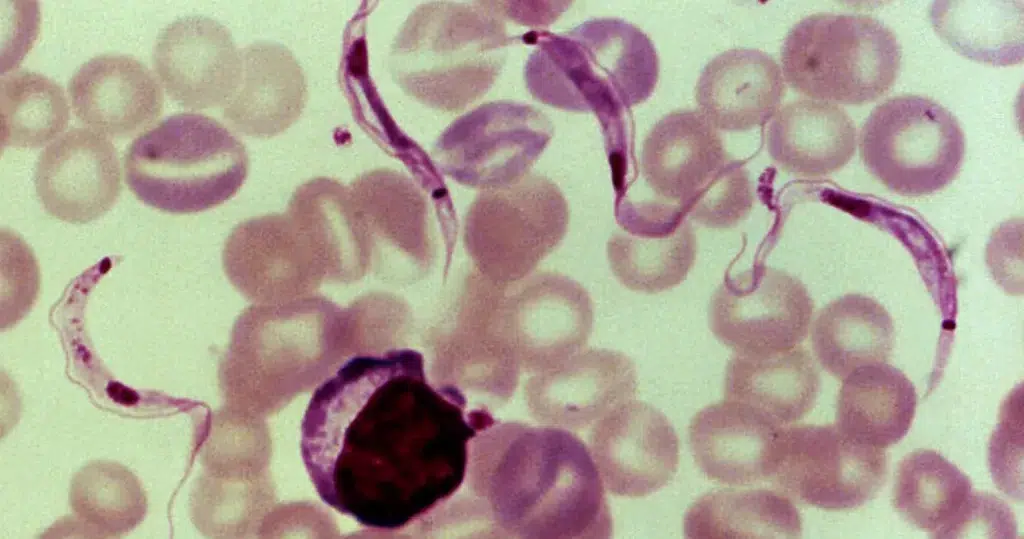
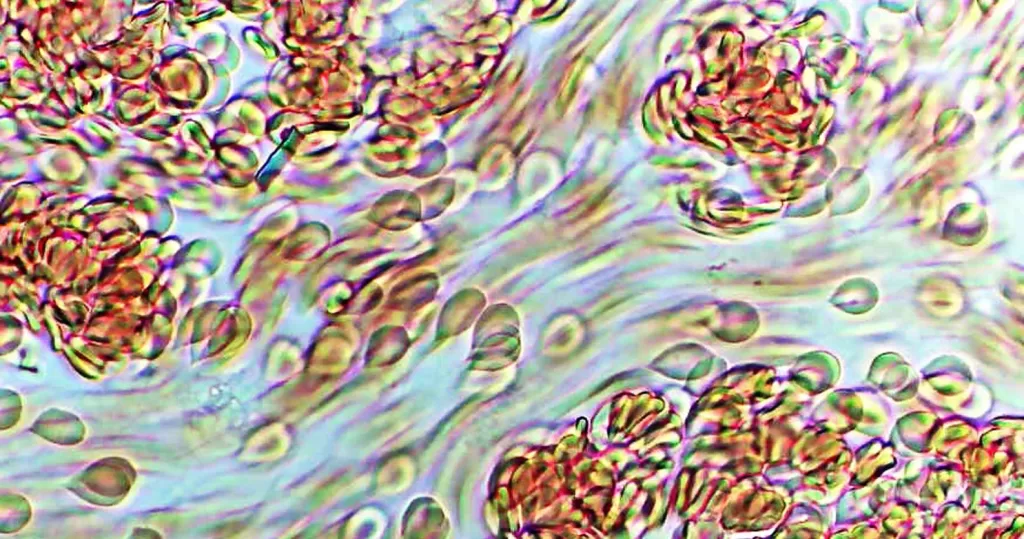
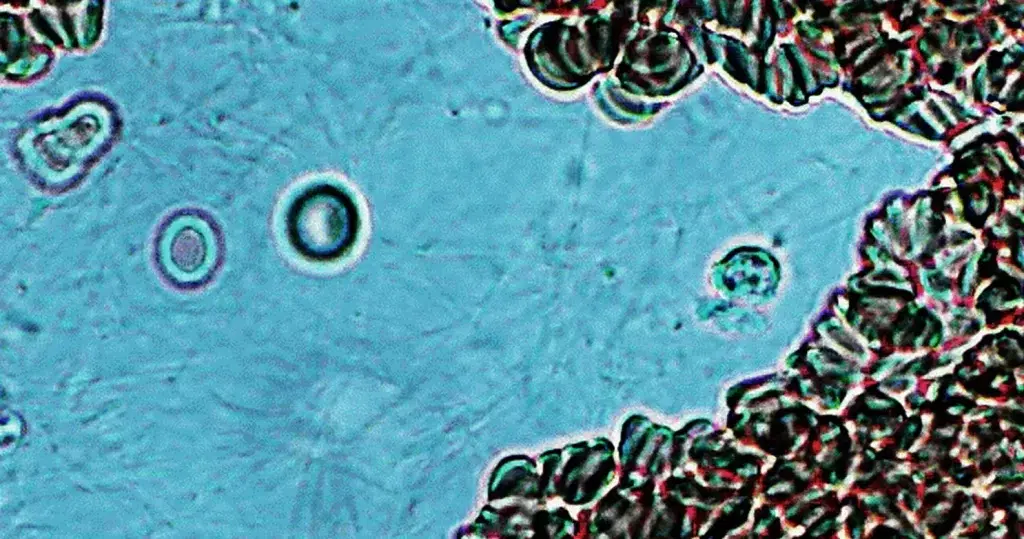
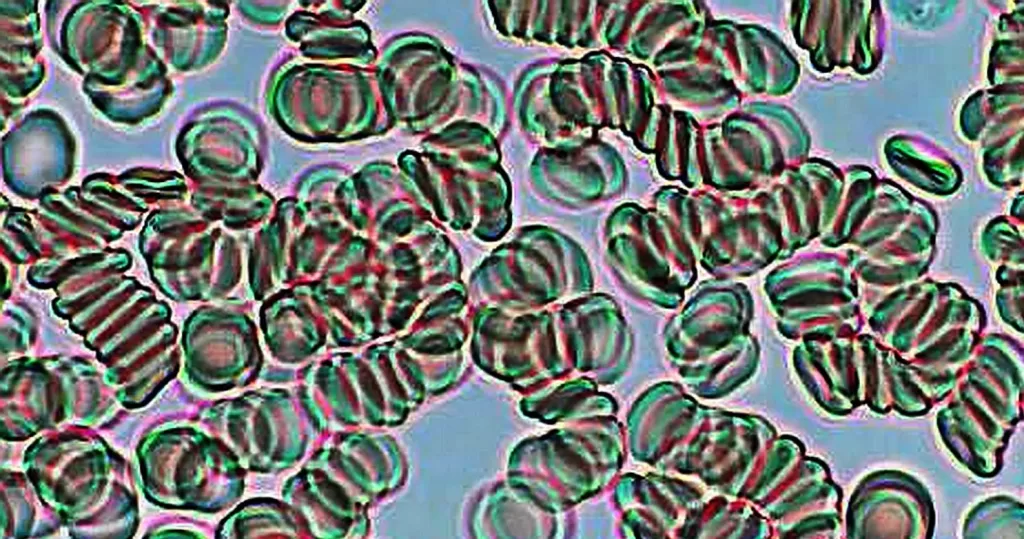
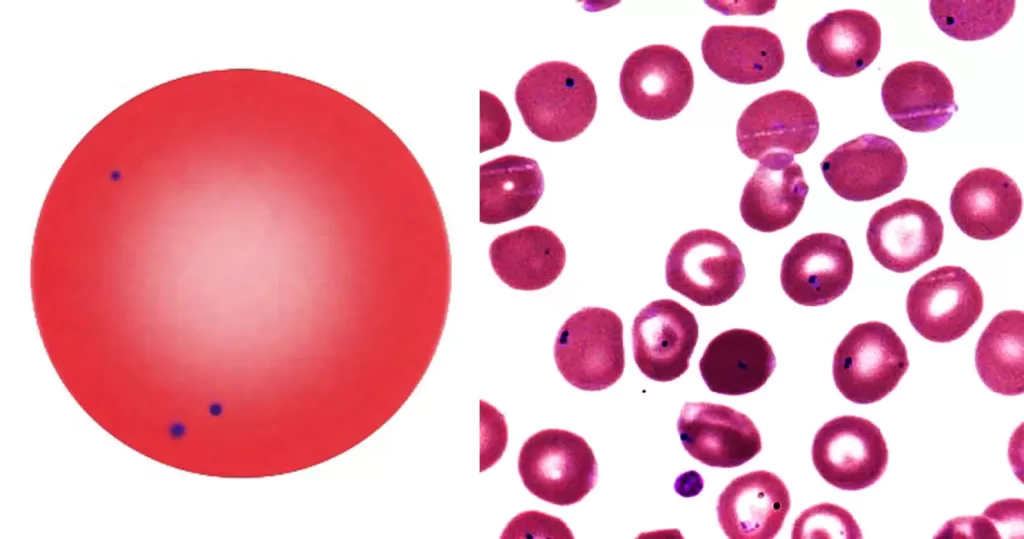
Use of Stains: The blood smear is stained to enhance the visibility of the cells. The most common stains used are Wright’s stain or Giemsa stain. These stains allow differentiation between the various types of white blood cells based on their cytoplasm and nuclear characteristics.- Wright’s Stain: A Romanowsky-type stain that consists of eosin and methylene blue. It stains eosinophilic (acidic) granules and basophilic (basic) granules, while also highlighting the nuclear morphology of cells.
- Giemsa Stain: Used for more detailed examination, especially of the nuclear structure and morphology of leukocytess.
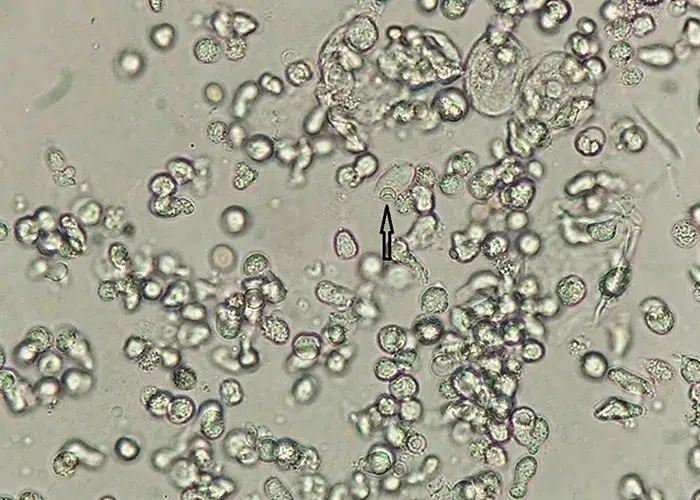
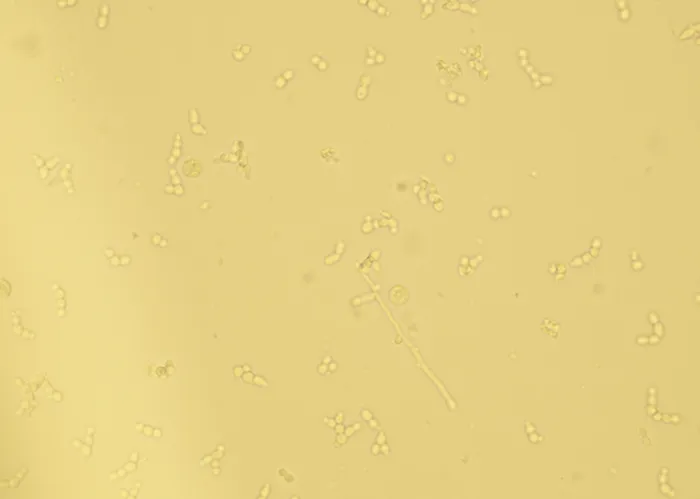
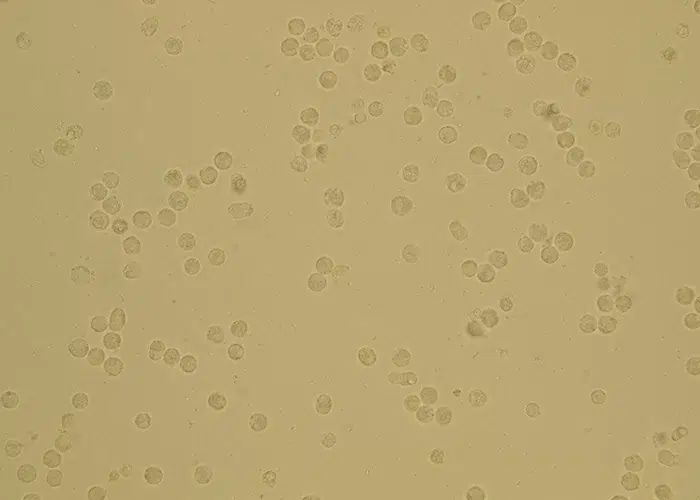
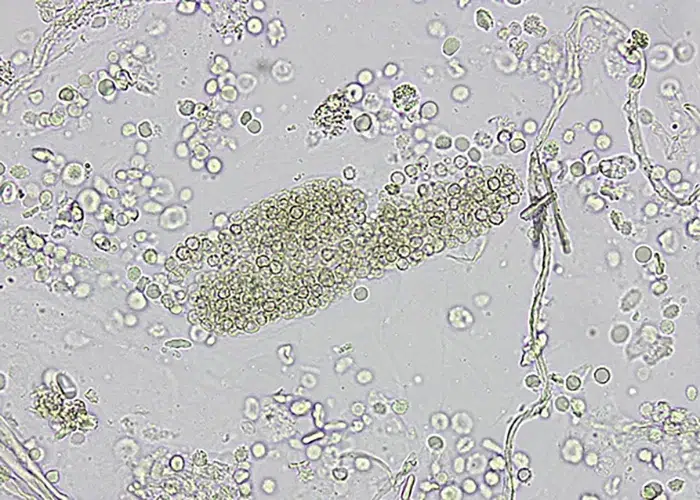
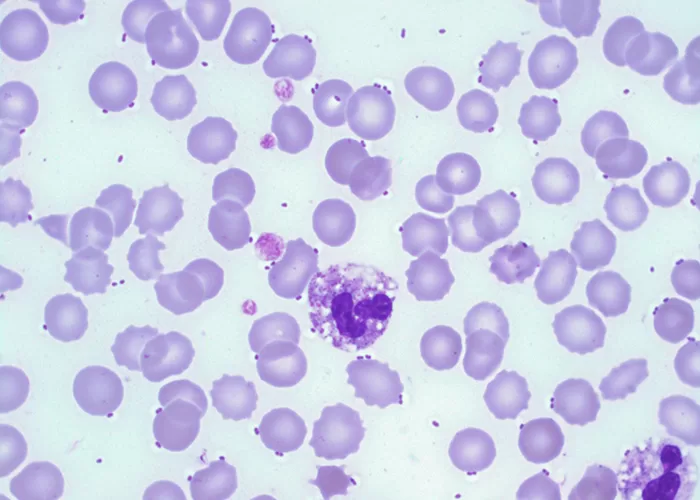
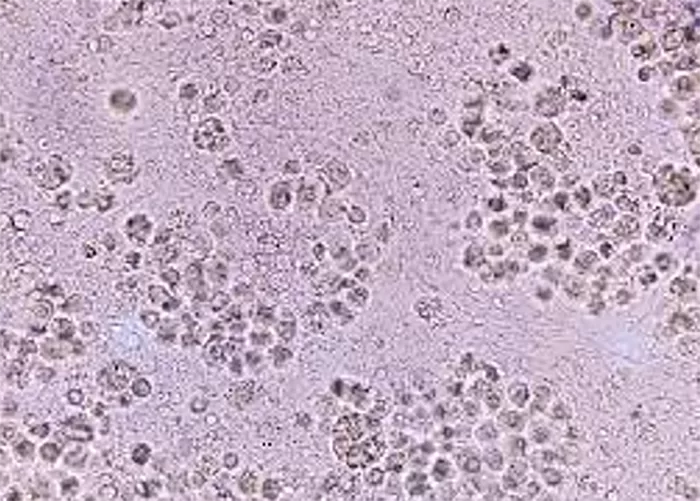
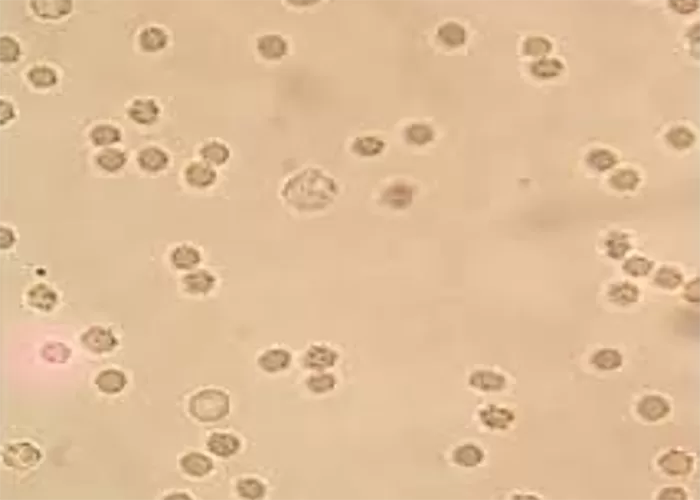
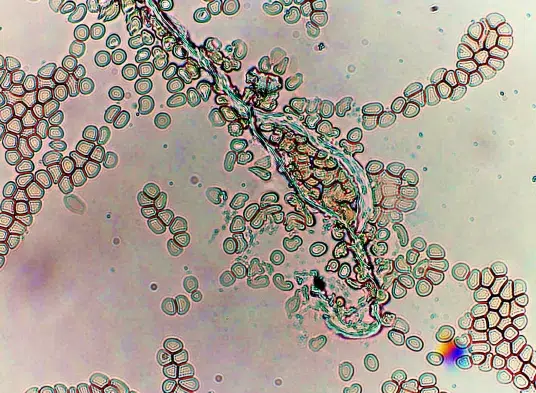
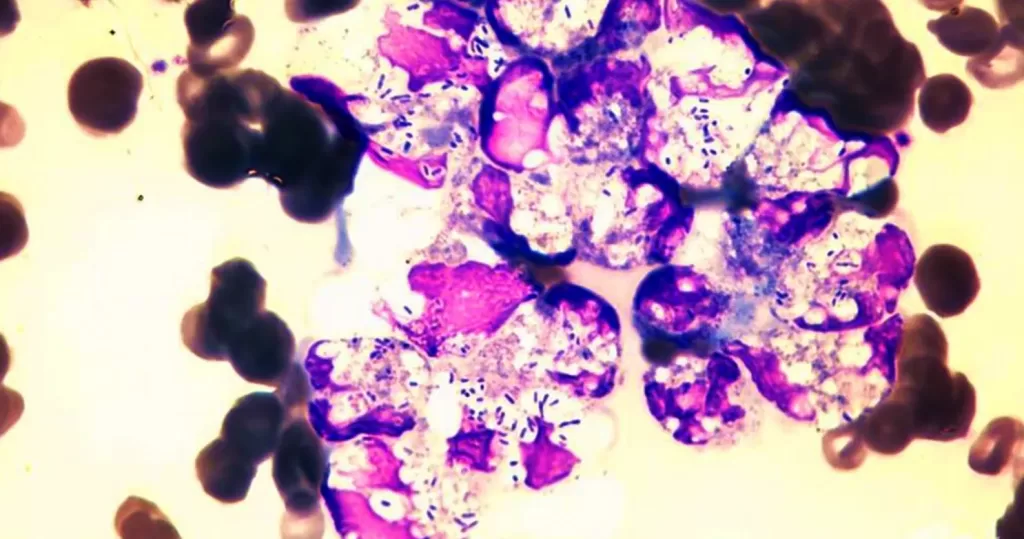
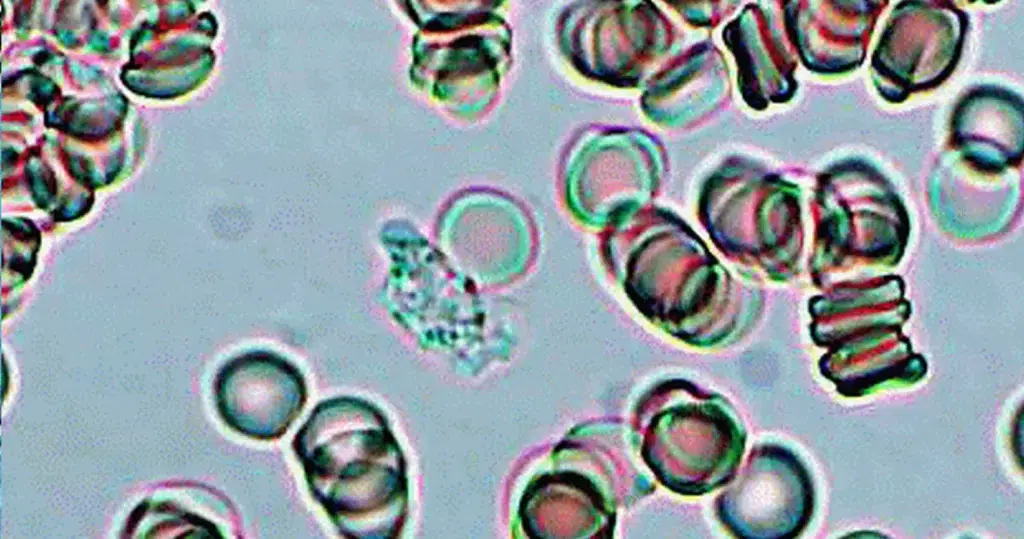
- Microscopic Examination: Examine Under a Microscope:
- The stained blood smear is examined under an oil immersion microscope, usually at a magnification of 1000x.
- Identify the leukocytes Types: The technician visually identifies and classifies the different types of white blood cells. The major leukocytes types are:
- Neutrophils (segmented or band-shaped nuclei)
- Lymphocytes (round nuclei with a high nuclear-to-cytoplasmic ratio)
- Monocytes (larger cells with a kidney-shaped nucleus)
- Eosinophils (bilobed nucleus and red granules in the cytoplasm)
- Basophils (lobed nucleus and blue granules in the cytoplasm)
- Count the leukocytes Types: The technician counts a total of 100 white blood cells and classifies them into one of these five types, typically recording the results as a percentage of the total.
- Calculating the Differential Count:
- Record the Percentage: After counting at least 100 cells, the technician calculates the percentage of each leukocytes type observed. For example, if 50 out of 100 cells are neutrophils, the neutrophil percentage is 50%.
- Absolute Count (Optional): In some cases, an absolute leukocytes count is also calculated by multiplying the percentage of each leukocytes type by the total leukocytes count (which can be determined via an automated hematology analyzer).
- Reporting the Results: The results are usually expressed in two ways:
- Percentage: The percentage of each type of leukocytes relative to the total.
- Absolute Count: The number of each type of leukocytes per unit of blood (e.g., per microliter or liter).
Automated Differential Count (Alternative Method):
In modern laboratories, automated hematology analyzers are frequently used to count and differentiate white blood cells. These devices use flow cytometry and other technologies to identify WBC types and provide a numerical breakdown. However, manual microscopic examination remains a gold standard for detailed analysis, especially when abnormalities or complex cases are suspected.
A detailed breakdown of potential interpretations for each leukocytes type:
Neutrophils
- Normal Range: 40-70% of total WBC count.
- Function: Neutrophils are the first responders to infection, especially bacterial infections.
Interpretation of Abnormal Results:
- Neutrophilia (Increased Neutrophils)
Possible Causes:
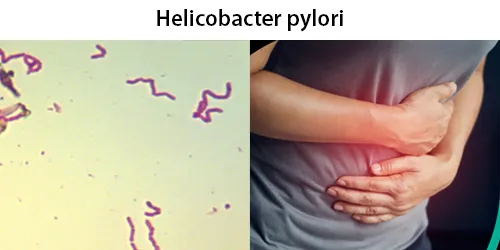
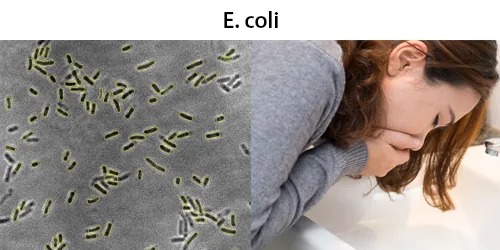
- Bacterial infections (e.g., pneumonia, sepsis, abscesses).
- Inflammatory conditions (e.g., rheumatoid arthritis, inflammatory bowel disease).
- Acute stress responses (e.g., physical trauma, burns, surgery).
- Chronic myelogenous leukemia (CML) or other myeloproliferative disorders.
- Tissue necrosis (e.g., myocardial infarction, burns).
- Steroid therapy: Can induce a relative neutrophilia due to demargination of neutrophils.
- Neutropenia (Decreased Neutrophils)
Possible Causes:
- Viral infections (e.g., hepatitis, HIV).
- Bone marrow disorders (e.g., aplastic anemia, leukemia).
- Chemotherapy or radiation therapy: Which suppress bone marrow activity.
- Autoimmune diseases (e.g., systemic lupus erythematosus).
- Severe bacterial infections (can lead to neutropenia in severe cases).
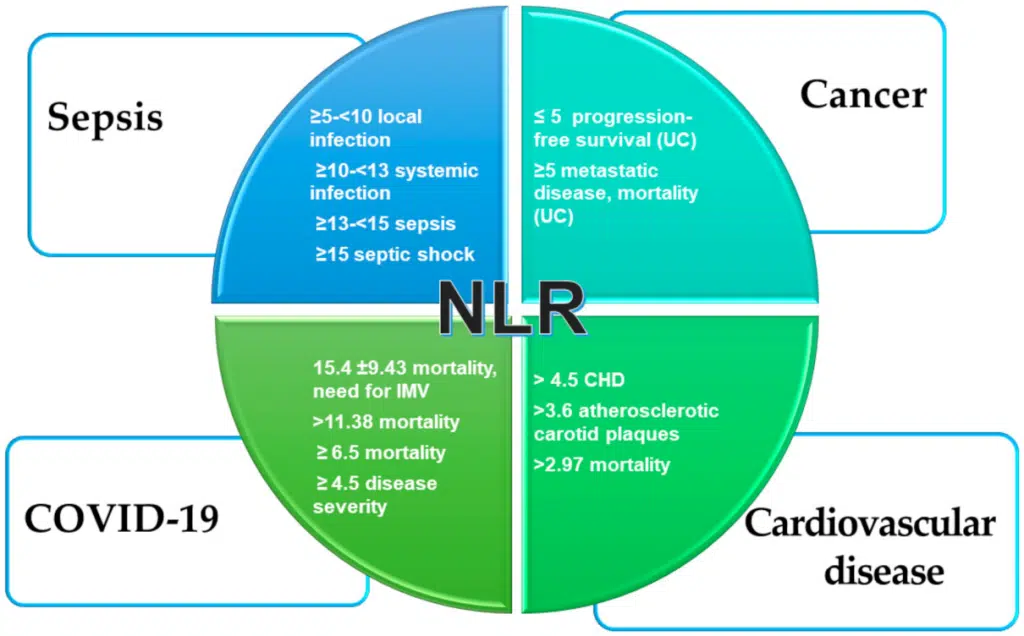
Lymphocytes
- Normal Range: 20-40% of total WBC count.
- Function: Lymphocytes play a key role in adaptive immunity, with B-cells producing antibodies and T-cells involved in cell-mediated immunity.
Interpretation of Abnormal Results:
- Lymphocytosis (Increased Lymphocytes)
Possible Causes:
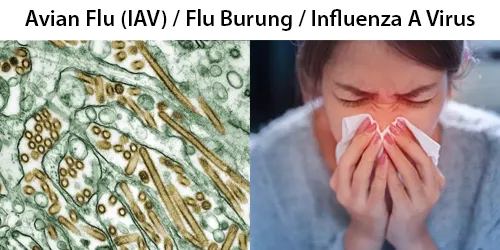
- Viral infections (e.g., Epstein-Barr virus, cytomegalovirus, influenza).
- Chronic lymphocytic leukemia (CLL) or other lymphoproliferative disorders.
- Acute viral infections (e.g., chickenpox, mumps).
- Autoimmune conditions (e.g., rheumatoid arthritis, thyroiditis).
- Lymphopenia (Decreased Lymphocytes)
Possible Causes:
- Acute bacterial infections (e.g., sepsis).
- HIV/AIDS (which affects T-cells specifically).
- Corticosteroid use: Steroids can reduce lymphocyte levels.
- Chemotherapy or radiation: Suppresses lymphocyte production in the bone marrow.
- Severe malnutrition or immunodeficiency diseases.
Monocytes
- Normal Range: 2-8% of total WBC count.
- Function: Monocytes differentiate into macrophages in tissues, which help with phagocytosis of pathogens and dead cells.
Interpretation of Abnormal Results:
- Monocytosis (Increased Monocytes)
Possible Causes:
- Chronic infections (e.g., tuberculosis, brucellosis).
- Chronic inflammatory diseases (e.g., inflammatory bowel disease, rheumatoid arthritis).
- Leukemias (especially monocytic or myelomonocytic leukemias).
- Post-infection recovery: Monocytes increase in the recovery phase of bacterial infections.
- Myelodysplastic syndromes or myeloproliferative disorders.
- Monocytopenia (Decreased Monocytes)
Possible Causes:
- Bone marrow failure (e.g., aplastic anemia).
- Corticosteroid use.
- Acute infections (can suppress monocyte production).
Eosinophils
- Normal Range: 1-4% of total WBC count.
- Function: Eosinophils are involved in allergic reactions and defense against parasitic infections.
Interpretation of Abnormal Results:
- Eosinophilia (Increased Eosinophils)
Possible Causes:
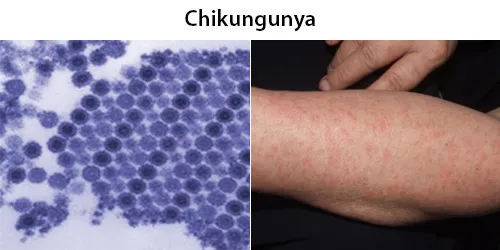
- Allergic reactions (e.g., asthma, hay fever, drug allergies).
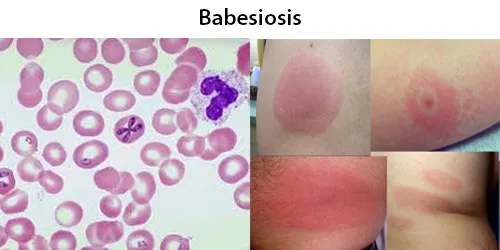
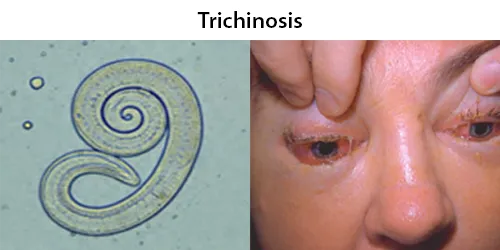
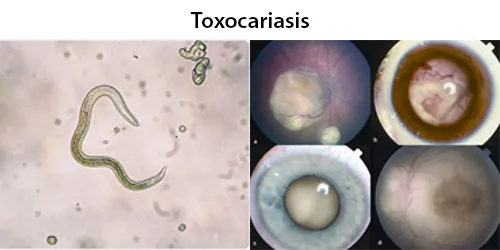
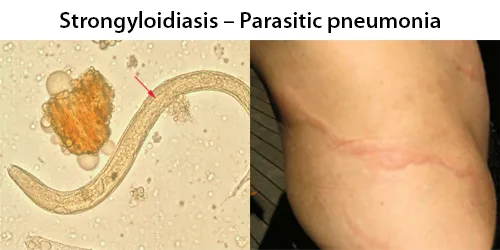
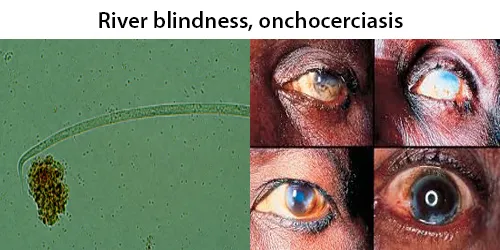
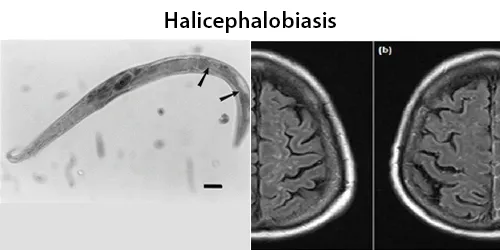
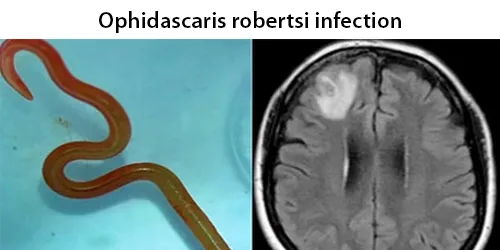
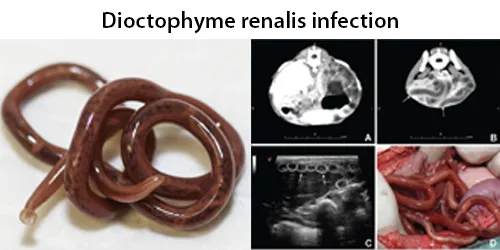
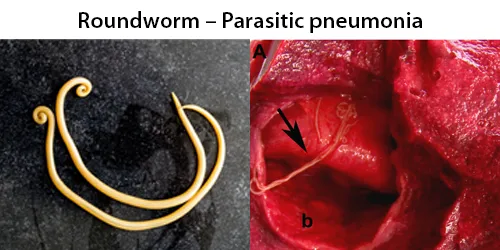
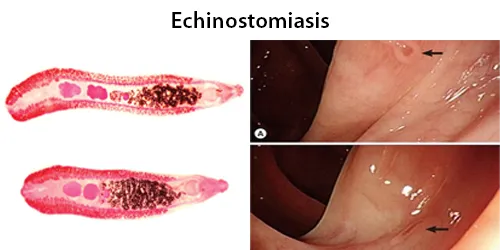
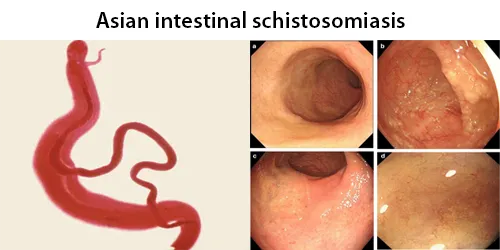
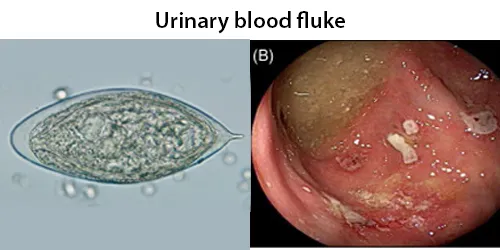
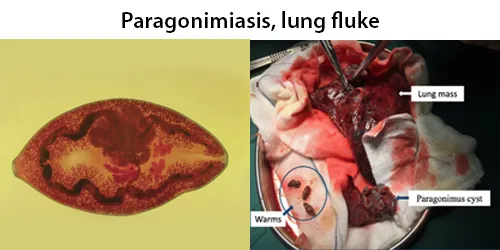
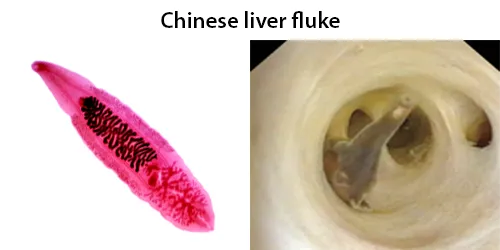
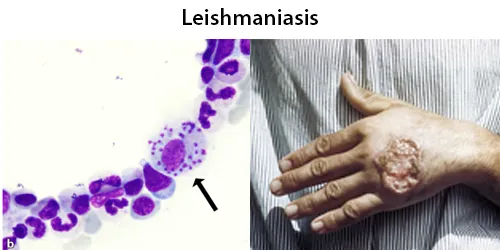
- Parasitic infections (e.g., hookworm, schistosomiasis).
- Autoimmune diseases (e.g., eosinophilic granulomatosis with polyangiitis).
- Skin conditions (e.g., eczema, psoriasis).
- Certain malignancies (e.g., Hodgkin’s lymphoma, some leukemias).
- Eosinopenia (Decreased Eosinophils)
Possible Causes:
- Corticosteroid therapy: Can suppress eosinophil production.
- Acute stress response: Typically, eosinophils decrease during stress or inflammation.
- Cushing’s syndrome or hypercortisolism.
Basophils
- Normal Range: 0-1% of total WBC count.
- Function: Basophils are involved in allergic responses and inflammation, releasing histamine and other chemicals.
Interpretation of Abnormal Results:
- Basophilia (Increased Basophils)
Possible Causes:
- Allergic reactions (e.g., allergic rhinitis, anaphylaxis).
- Chronic myeloproliferative disorders (e.g., chronic myelogenous leukemia).
- Hypothyroidism.
- Infections (e.g., tuberculosis, chickenpox).
- Ulcerative colitis or other chronic inflammatory conditions.
- Basopenia (Decreased Basophils)
Possible Causes:
- Acute infections or stress can cause basophils to decrease.
- Hyperthyroidism.
- Corticosteroid therapy can lead to a drop in basophil numbers.
Key Considerations in Interpretation:
- Contextual Factors: Clinical symptoms, medical history, and other laboratory results are essential for proper interpretation. For instance, an increase in neutrophils (neutrophilia) is most likely due to a bacterial infection, while an increase in lymphocytes (lymphocytosis) often suggests a viral infection.
- Age and Other Factors: The interpretation may vary based on age, medical treatments, or the presence of other underlying conditions. For example, newborns typically have a higher neutrophil count than adults.